Medicine and Health
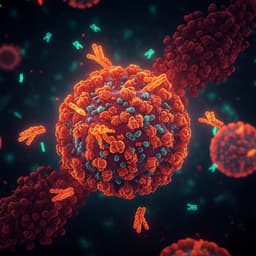
Exhaled aerosols among PCR-confirmed SARS-CoV-2-infected children
T. S. Murray, J. Sznitman, et al.
This prospective study led by Thomas S Murray, Josue Sznitman, and others reveals intriguing findings about aerosol concentrations in SARS-CoV-2 PCR-positive and -negative children and adolescents. The research highlights that vaccination status emerges as a significant predictor, while children show no signs of superspreading, challenging common perceptions around transmission in younger populations.
Playback language: English
Related Publications
Explore these studies to deepen your understanding of the subject.