Medicine and Health
Engineered ACE2 decoy mitigates lung injury and death induced by SARS-CoV-2 variants
L. Zhang, S. Dutta, et al.
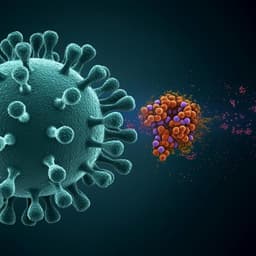
The study addresses the urgent need for COVID-19 therapeutics that retain efficacy against SARS-CoV-2 variants of concern. Despite effective vaccines, hesitancy, limited access, breakthrough infections, and VOCs with mutations that increase ACE2 affinity and enable immune escape diminish current protections. Monoclonal antibodies targeting spike can lose neutralization potency against certain variants. Soluble ACE2 (sACE2) can serve as a decoy receptor, but wild-type sACE2 showed limited clinical benefit and in vivo neutralization when used as an Fc fusion. Prior deep mutagenesis identified ACE2 variants with enhanced spike affinity; a triple mutant (v2.4: T27Y, L79T, N330Y) bound spike ~35-fold tighter and neutralized on par with high-affinity mAbs in vitro. The research question is whether an engineered ACE2 decoy with enhanced affinity demonstrates in vivo efficacy to prevent viral entry, ameliorate lung vascular injury/ARDS, and reduce mortality across SARS-CoV-2 variants using a human ACE2 transgenic mouse model.
The spike (S) protein mediates ACE2-dependent entry; many therapeutic mAbs bind S epitopes with sub-nanomolar affinity but often show reduced activity against VOCs. Clinical and preclinical experiences with wild-type sACE2 show improved oxygenation but no mortality benefit and limited in vivo neutralization as an Fc-fusion, motivating development of next-generation ACE2 derivatives. Prior engineering efforts (deep mutagenesis) produced ACE2 variants with improved S binding (e.g., v2.4). K18-hACE2 transgenic mice model severe SARS-like lung injury due to human ACE2 expression, enabling evaluation of antivirals’ effects on endothelial barrier integrity, edema, and survival.
- Molecular dynamics (MD) simulations and modeling: Approximately 400 µs of all-atom MD for apo ACE2 (WT and v2.4) and ~530 µs for RBD-bound complexes (original/Wuhan), plus ~10 µs for Delta and Gamma RBD-bound systems. Time-lagged independent component analysis (TICA) and Markov state models (MSMs) characterized interfacial dynamics. Features included interresidue distances at the ACE2–RBD interface; bootstrapping quantified uncertainty.
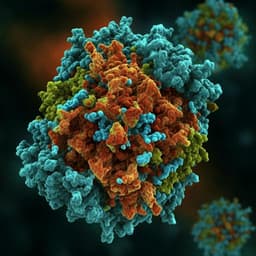
- Protein engineering: Engineered sACE2 v2.4 carries T27Y, L79T, N330Y. Constructs included monomeric sACE2 (aa 19–615, His-tag), dimeric sACE2(aa 19–732)-IgG1 Fc fusions, and WT comparators. Proteins were expressed in Expi293F or ExpiCHO-S cells and purified via affinity and size exclusion chromatography.
- Pharmacokinetics (PK) and toxicology in mice: CD-1 or C57BL/6 mice received sACE2 v2.4 (0.5 mg/kg IV) or sACE2 v2.4-IgG1 (2.0 mg/kg IV). Serum levels measured by ACE2 ELISA, IgG1 ELISA, and ACE2 catalytic activity; immunoblotting assessed proteolysis. Alternative routes included intratracheal instillation (1.0 mg/kg) and inhalation. Toxicology assessed weight, CBC, serum chemistry, and histopathology.
- Mouse infection models: K18-hACE2 mice (8–10 weeks) inoculated intranasally with live SARS-CoV-2 WA-1/2020 or P.1 (Gamma) at 1×10^4–1×10^6 PFU. Outcomes included survival, weight, lung vascular permeability (Evans blue–albumin, EBA), lung wet/dry ratio (edema), endothelial cell loss (flow cytometry), VE-cadherin expression (qPCR), histology, fibrosis staining, and viral burden (qPCR for S and NSP; plaque-forming assay).
- Treatment regimens: Prophylaxis: single IV dose of sACE2 v2.4-IgG1 (10 mg/kg) 12 h pre-inoculation. Therapy: sACE2 v2.4-IgG1 IV daily for 7 days, starting 12 h (10 mg/kg) or 24 h (15 mg/kg) post-inoculation.
- Pseudovirus entry assays: rVSV-luciferase pseudovirus bearing SARS-CoV-2 S (MOI 0.1) used in A549, hACE2-A549, and primary human lung microvascular endothelial cells. Cells preincubated with sACE2-IgG1 WT or v2.4-IgG1 (5 or 25 µg/ml). In vivo pseudovirus assay: K18-hACE2 mice pretreated with 10 mg/kg sACE2-IgG1 (WT) or v2.4-IgG1 30 min before intraperitoneal pseudovirus (10^6 PFU); luciferase activity measured in organs at 24 h.
- Binding assays to S variants: Flow cytometry measured binding of monomeric sACE2 and dimeric sACE2-IgG1 (WT vs v2.4) to cells expressing full-length trimeric S from Wuhan, Alpha, Beta, Gamma, Delta, Epsilon, Lambda, and SARS-CoV-1. Comparison included EUA mAbs (REGN10933, REGN10987, VIR-7831, LY-CoV555). Biolayer interferometry (BLI) measured monovalent affinities to RBDs (Delta and Gamma).
- Disease in K18-hACE2 mice: WA-1/2020 at 1×10^6 PFU induced mortality starting day 5; 1×10^5 PFU starting day 7. P.1 (1×10^6 PFU) caused death 2 days earlier than WA-1/2020. Significant body weight loss, increased lung vascular permeability (EBA), increased lung wet/dry ratio (edema), endothelial cell loss (~one-third by day 7), reduced VE-cadherin, pulmonary hemorrhage, immune infiltration, and collagen deposition observed. P.1 lung viral mRNA (S and NSP) on day 6 was ~5-fold higher than WA-1/2020 on day 7.
- MD mechanism: v2.4 mutations stabilized new polar interactions with RBD loops (ACE2 v2.4 Y27–RBD Y473; ACE2 v2.4 Y330–RBD P499 backbone), yielding single-peaked hydrogen bond distance distributions (~4 Å) and reduced RBD loop fluctuations, consistent with enhanced affinity.
- PK/tox: Monomeric sACE2 v2.4 had a serum half-life <10 min (mouse). sACE2 v2.4-IgG1 persisted by human IgG1 ELISA for ≥7 days, but ACE2 moiety was cleared within 24 h in mice; proteolysis to long-lived IgG1 fragments in mouse serum but resistant in human serum. Intratracheal/inhaled delivery produced high, stable lung levels for hours with minimal plasma detection. No evident toxicity at tested doses.
- In vitro entry inhibition: sACE2 v2.4-IgG1 produced ~5-fold greater inhibition of pseudovirus entry than WT sACE2-IgG1 across hACE2-A549, A549, and hLMVECs.
- In vivo pseudovirus: Pretreatment with 10 mg/kg sACE2 v2.4-IgG1 significantly reduced lung luciferase signals compared to WT sACE2-IgG1 and buffer; lungs showed highest baseline entry vs other organs.
- Prophylaxis (WA-1/2020, 1×10^4 PFU): Single 10 mg/kg IV dose 12 h before challenge led to 100% survival with stable or increased body weight; PBS controls died by day 8 with ~30% weight loss. Lung EBA permeability and wet/dry ratio were not significantly elevated, indicating protection from ARDS.
- Therapy (WA-1/2020, 1×10^4 PFU): Daily IV sACE2 v2.4-IgG1 starting 12 h (10 mg/kg) or 24 h (15 mg/kg) post-inoculation improved 14-day survival to ~50–60% vs 0% in controls, attenuated weight loss, reduced EBA permeability and edema at day 7, and eliminated lung viral gene expression by day 7. In survivors, permeability and edema normalized by day 14; histology showed reduced immune infiltration.
- Breadth of binding: sACE2 v2.4 (monomer and dimer) showed increased binding to S from Wuhan, Alpha, Beta, Gamma, Delta, Epsilon, Lambda, and bound SARS-CoV-1 S. Binding was comparable to or broader than several clinical mAbs; some mAbs (e.g., REGN10933, LY-CoV555) showed variable reduced binding to certain VOCs. sACE2 v2.4-IgG1 and REGN10933 induced S1 shedding at high concentrations. BLI showed tight monovalent affinities for Delta and Gamma RBDs (VIR-7831 and sACE2 v2.4 among the tightest).
- P.1 (Gamma) therapy: Early treatment (12 h start) improved survival to ~50–60%; delayed treatment (24 h start) prolonged time to death but did not significantly improve survival. Both regimens markedly reduced EBA permeability and edema at day 6. Early treatment reduced lung viral plaque-forming capacity by ~80% on day 6 and decreased viral transcripts more than delayed treatment. Surviving mice returned to near-baseline vascular permeability by day 14 with reduced immune infiltration.
The engineered sACE2 v2.4-IgG1 decoy effectively prevents viral entry by competing with native ACE2 and demonstrates robust mitigation of lung endothelial injury, edema, and mortality in a stringent K18-hACE2 model. Molecular simulations explain enhanced affinity via stabilizing interactions with RBD loops. Despite immune escape undermining many mAbs and reduced vaccine efficacy against VOCs, sACE2 v2.4-IgG1 maintains tight binding across multiple variants and even SARS-CoV-1, suggesting resilience to antigenic drift within ACE2-dependent coronaviruses. Timing of therapy is critical: early intervention (12 h) yields substantial survival benefits, whereas later initiation (24 h) still reduces lung injury and viral load but may not overcome downstream inflammatory pathology for highly virulent variants like P.1. PK data suggest complementary delivery strategies: local inhalational dosing early in infection for high lung exposure, followed by systemic IV dosing for disseminated disease. These findings support sACE2 v2.4-IgG1 as a broadly active therapeutic candidate with multiple potential mechanisms (decoy function and ACE2 enzymatic activity) to counter SARS-CoV-2-induced ARDS.
An engineered ACE2 decoy (sACE2 v2.4-IgG1) with enhanced spike affinity provides broad protection against SARS-CoV-2 variants in vivo. It prevents viral entry, protects the lung endothelial barrier, mitigates ARDS, and significantly improves survival in K18-hACE2 mice challenged with WA-1/2020 and P.1 variants. Binding breadth comparable to effective mAbs and activity against SARS-CoV-1 highlight its potential resilience to variant evolution. Future work should optimize dosing and delivery routes (including inhalation), evaluate efficacy at different disease stages, and validate translational potential in non-human primate models and ultimately clinical trials.
- Translational modeling: Mouse disease kinetics may not directly mirror human COVID-19 progression, complicating the mapping of treatment windows.
- Timing sensitivity: Delayed initiation (24 h) for the more virulent P.1 variant reduced pathology and viral load but did not significantly improve survival, indicating a narrow therapeutic window and possible contributions from irreversible inflammatory damage.
- Species-specific PK: Rapid proteolysis of the ACE2 moiety in mouse serum (contrasting stability in human serum) may limit interpretation of exposure-response relationships in mice.
- Scope of in vivo testing: Efficacy was demonstrated in K18-hACE2 mice for two variants; broader in vivo validation (e.g., non-human primates), dose-ranging, and alternative delivery routes were not fully explored.
Related Publications
Explore these studies to deepen your understanding of the subject.