Medicine and Health
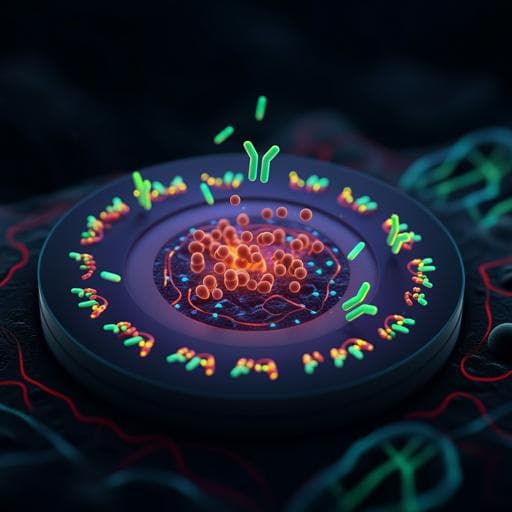
E-DNA scaffold sensors and the reagentless, single-step, measurement of HIV-diagnostic antibodies in human serum
C. Parolo, A. S. Greenwood, et al.
This groundbreaking research by Claudio Parolo, Ava S. Greenwood, Nathan E. Ogden, Di Kang, Chase Hawes, Gabriel Ortega, Netzahualcóyotl Arroyo-Currás, and Kevin W. Plaxco unveils the remarkable potential of E-DNA scaffold sensors for rapid, multiplexed antibody measurement at the point of care. With a focus on three HIV-specific antibodies, these innovative sensors challenge traditional methods by blending the precision of ELISA with the convenience of modern testing.
Related Publications
Explore these studies to deepen your understanding of the subject.