Biology
Dietary supplementation with biogenic selenium nanoparticles alleviate oxidative stress-induced intestinal barrier dysfunction
L. Qiao, X. Zhang, et al.
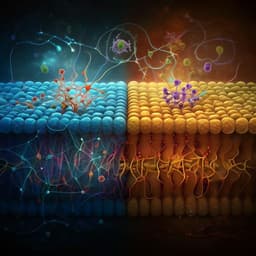
The study addresses how dietary selenium, particularly biogenic selenium nanoparticles (SeNPs), influences oxidative stress-related intestinal barrier dysfunction, with a focus on mitochondrial function and gut microbiota. Selenium is essential for antioxidant defense through selenoproteins such as glutathione peroxidase (GPx) and thioredoxin reductase (TrxR). Se deficiency is prevalent in many regions and is linked to diseases, including intestinal disorders. The intestine is highly susceptible to oxidative stress, with mitochondrial ROS playing a key role in epithelial injury and barrier dysfunction. Prior evidence suggests Se supports mitochondrial structure/function and biogenesis, reducing ROS and preserving membrane potential. Se status also correlates with inflammatory bowel disease severity, but inorganic Se has higher toxicity and lower bioavailability compared with SeNPs. The authors hypothesized that dietary SeNPs protect intestinal barrier integrity via redox regulation and microbiota modulation. They compared different SeNPs doses (0.0, 0.3, 0.6 mg/kg) on barrier function, mitochondrial structure/function, and gut microbiota in mice, and used fecal microbiota transplantation (FMT) to test whether SeNPs-driven microbiota changes mediate protection independently of Se itself.
Background highlights include: (1) Se exerts biological effects via 25+ selenoproteins, notably GPx and TrxR, which maintain redox homeostasis. (2) Se deficiency is associated with cardiomyopathy, Keshan disease, intestinal disease, neurological disorders, and is common in certain regions. (3) IBD patients (UC and CD) often present with reduced serum Se levels, inversely correlated with disease activity; Se has been proposed as a biomarker. (4) Inorganic Se forms have higher toxicity and lower bioavailability; SeNPs offer lower toxicity with effective bioactivity and can upregulate antioxidant enzymes. (5) Prior work showed L. casei ATCC 393-synthesized SeNPs alleviate diquat-induced epithelial barrier dysfunction in vitro; dietary Se also modulates gut microbiota composition, which can reciprocally affect Se bioavailability and selenoprotein expression. (6) Se supports mitochondrial integrity and biogenesis, reducing ROS and preserving membrane potential. These findings motivated testing SeNPs as a dietary intervention to protect the intestinal barrier via mitochondrial and microbiota mechanisms.
Reagents: Biogenic SeNPs synthesized by Lactobacillus casei ATCC 393 as per prior methods. Diquat (oxidative stress inducer) was used for acute exposure (25 mg/kg i.p.). Multiple commercial kits were used for antioxidant enzymes, oxidative damage markers, ELISAs (IL-1β, IL-18, sIgA, 8-OHdG), mitochondrial function (ATP, MMP), ROS detection (DHE), and Western blots (Nrf2, NQO1, HO-1, ZO-1, occludin, claudin1, NLRP3, ASC, caspase-1, IL-1β, IL-18). Selenium content was measured by ICP-MS. Animals and diets: Male C57BL/6 mice. Experimental diets: Se-deficient (0.0-Se; actual 0.009 mg/kg), SeNPs-supplemented 0.3-Se (0.320 mg/kg) and 0.6-Se (0.603 mg/kg). Drinking water and saline contained no Se. All procedures approved by IACUC. Experimental design:
- Experiment I: 72 mice (3 weeks old) randomized to 0.0-Se, 0.3-Se, 0.6-Se diets for 10 weeks (ad libitum). Two weeks before end, feces collected for FMT donors. Twelve hours before sacrifice, half of each group received diquat 25 mg/kg i.p.; others received PBS. Four hours prior to end, mice were gavaged with FITC-dextran (4 kDa, 400 mg/kg) to assess permeability.
- Experiment II (FMT): 40 mice (6 weeks old) assigned to control, diquat model, 0.0-Se-FMT+diquat, 0.6-Se-FMT+diquat (n=10/group). The two FMT groups received an antibiotic cocktail in drinking water for 8 weeks (clindamycin, metronidazole, penicillin, vancomycin and/or neomycin), then 7 weeks of daily gavage with 200 µL fecal transplant material from 0.0-Se or 0.6-Se donors. Diquat exposure applied afterward to induce oxidative injury. Assays and analyses:
- Intestinal barrier function: Serum FITC-dextran, serum DAO and D-lactate; Western blots for tight junction proteins (ZO-1, occludin, claudin-1); histology (H&E) for villus morphology; AB-PAS for goblet cells; qPCR for mucin MUC2 and antimicrobial peptide REG3G.
- Antioxidant capacity: Jejunal T-AOC, SOD, GPx, TrxR activities; MDA as lipid peroxidation marker.
- Mitochondrial function: Jejunal ROS by DHE; transmission electron microscopy (TEM) of mitochondrial ultrastructure; mitochondrial ATP (luminescence), membrane potential (JC-1 Red/Green), 8-OHdG; mtDNA copy number by qPCR (COX2/HK2 ratio); mRNA of TFAM, POLG, POLG2.
- Inflammation signaling: Western blots for NLRP3 inflammasome components (NLRP3, ASC, pro/cleaved caspase-1) and cytokines (IL-1β, IL-18); Nrf2 pathway (total and nuclear Nrf2, HO-1, NQO1).
- Microbiota: 16S rRNA V3–V4 sequencing (Illumina MiSeq, QIIME); alpha diversity (ACE, Chao1, Shannon, Simpson), beta diversity and PCoA; taxonomic shifts at phylum/genus; Firmicutes/Bacteroidetes ratio; functional prediction by PICRUSt2 with KEGG; SCFAs in cecal content quantified by GC-MS (acetate, propionate, butyrate, isobutyrate, isovalerate, valerate, caproate; total SCFAs). Correlation heatmaps (Spearman) between genera and biochemical indices. Statistics: Data mean ± SEM. One-way ANOVA with post hoc tests for multiple comparisons; Student’s t-test for two-group comparisons. P<0.05 considered significant.
- Growth and Se status: After 10 weeks, mice on 0.6-Se had higher final body weight vs 0.0-Se; feed conversion rate (FCR) was significantly lower in 0.3-Se and 0.6-Se vs 0.0-Se, lowest in 0.6-Se. Tissue Se content (liver, kidney, serum, small intestine) increased with SeNP supplementation (n=10; P<0.05 to P<0.001).
- Barrier integrity: Diquat increased intestinal permeability (serum FITC-dextran) and injury markers (DAO, D-lactate) and reduced tight junction proteins (ZO-1, occludin, claudin-1). Se deficiency exacerbated damage; 0.6-Se supplementation markedly mitigated diquat-induced barrier dysfunction (n≈6–8; P<0.05 to P<0.001). Histology showed villus injury with diquat worsened by 0.0-Se, while 0.6-Se preserved morphology; goblet cell counts and jejunal MUC2 and REG3G mRNA were increased by 0.6-Se vs diquat and 0.0-Se groups.
- Antioxidant capacity and inflammation: Se deficiency reduced T-AOC, SOD, GPx, TrxR and increased MDA; diquat further aggravated oxidative stress. 0.6-Se significantly restored antioxidant indices and reduced MDA in jejunum (n=8). Pro-inflammatory cytokines IL-1β and IL-18 were elevated by Se deficiency and diquat; 0.6-Se reduced IL-1β/IL-18 and increased sIgA vs 0.0/0.3-Se under diquat; 0.3-Se often did not differ from 0.0-Se.
- Mitochondrial protection: Se deficiency increased ROS; diquat further increased ROS. 0.6-Se reduced jejunal ROS (DHE). TEM showed severe mitochondrial swelling and cristae loss in 0.0-Se (worse with diquat); 0.6-Se preserved intact membranes and cristae. Mitochondrial ATP and MMP decreased with Se deficiency and more with diquat; 0.6-Se restored both (n=8). 8-OHdG increased with 0.0-Se; 0.6-Se protected mtDNA from oxidative damage. mtDNA copy number was unchanged by SeNPs in controls but dose-dependently increased with SeNPs under diquat. Expression of mtDNA replication/biogenesis genes (TFAM, POLG, POLG2) was lower in chronic 0.0-Se vs 0.3/0.6-Se controls but paradoxically elevated in 0.0-Se under acute diquat; SeNPs attenuated this stress-induced upregulation.
- Nrf2/NLRP3 signaling: Se deficiency and diquat increased NLRP3 inflammasome (NLRP3, ASC, cleaved caspase-1) and IL-1β/IL-18; increasing dietary Se reduced these levels under diquat. SeNPs dose-dependently increased total and nuclear Nrf2 and downstream HO-1, NQO1 with or without diquat, indicating activation of antioxidant responses that suppress NLRP3 activation.
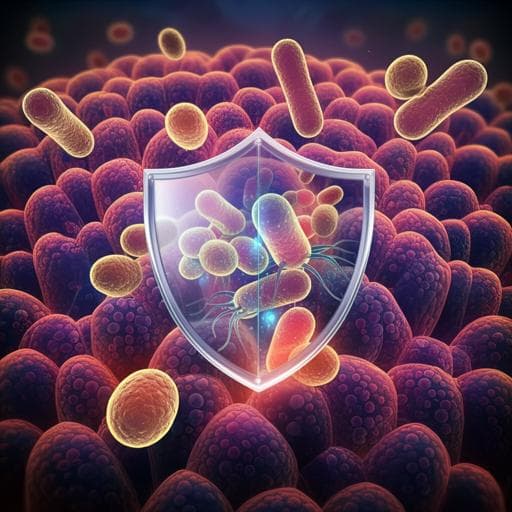
- Microbiota composition and metabolites: SeNPs did not change overall richness (ACE, Chao1) but increased diversity (higher Shannon, lower Simpson) at 0.6-Se vs 0.0-Se; PCoA showed distinct clustering. 0.6-Se increased Bacteroidetes and decreased Verrucomicrobia; showed a decreasing trend in Firmicutes/Bacteroidetes ratio. At genus level, 0.6-Se increased Bacteroides and Clostridium_XIVa and decreased Desulfovibrio. SCFAs in cecum increased with supranutritional Se (total SCFAs, butyrate, isobutyrate, valerate, isovalerate). Functional prediction showed enrichment in KEGG categories "Human Diseases" (level 1) and "Digestive system" (level 2) in 0.6-Se. Correlations: Helicobacter positively correlated with T-AOC, GPx, TrxR and sIgA; Bacteroides positively with sIgA and total SCFAs; Desulfovibrio negatively with total SCFAs, acetate, propionate. Se deficiency increased Desulfovibrio and decreased Bacteroides.
- FMT causality: Microbiota from 0.0-Se donors (0.0-Se-FMT) increased susceptibility to diquat-induced barrier dysfunction vs diquat alone, elevating permeability and reducing tight junction proteins; 0.6-Se-FMT conferred protection, improving villus height, goblet cells, and MUC2/REG3G expression. 0.6-Se-FMT restored antioxidant indices (higher T-AOC, SOD, GPx, TrxR; lower MDA), reduced IL-1β/IL-18, and increased sIgA vs diquat and 0.0-Se-FMT. Microbiota analysis: 0.0-Se-FMT increased F/B ratio and Desulfovibrio and reduced Candidatus_Saccharimonas and Rikenella; 0.6-Se-FMT decreased Desulfovibrio and increased Candidatus_Saccharimonas and Rikenella.
- FMT and mitochondria/signaling: 0.6-Se-FMT reduced jejunal ROS, preserved mitochondrial ultrastructure, increased ATP and MMP, lowered 8-OHdG, and rescued mtDNA copy number under diquat. It suppressed NLRP3 inflammasome activation and upregulated total/nuclear Nrf2, HO-1, NQO1 vs diquat and 0.0-Se-FMT, indicating microbiota-mediated activation of Nrf2 that inhibits mitochondrial dysfunction and inflammasome activation. Overall, dietary biogenic SeNPs and the derived microbiota protect against oxidative stress-induced intestinal barrier dysfunction via enhanced antioxidant defenses, mitochondrial protection, Nrf2 activation, NLRP3 inhibition, and favorable gut microbiota remodeling with increased SCFAs.
The findings support the hypothesis that dietary SeNPs protect the intestinal barrier during oxidative stress by modulating redox balance, mitochondrial function, and gut microbiota. Se deficiency compromises antioxidant capacity, increases ROS, and exacerbates mitochondrial damage, triggering NLRP3 inflammasome activation and pro-inflammatory cytokine release, which collectively disrupt tight junctions and mucus barrier. SeNP supplementation activates Nrf2 (elevated total and nuclear Nrf2, HO-1, NQO1), thereby reducing ROS and suppressing NLRP3 activation, preserving mitochondrial function (ATP, MMP, mtDNA integrity) and barrier integrity. SeNPs also beneficially remodel the gut microbiota (elevated Bacteroides and Clostridium_XIVa; reduced Desulfovibrio), increasing SCFA production that likely supports epithelial health. FMT experiments demonstrate that microbiota from SeNP-supplemented donors is sufficient to convey protection against diquat-induced damage and to activate Nrf2 while inhibiting NLRP3, implicating a microbiota–mitochondria–Nrf2 axis. Conversely, microbiota from Se-deficient donors increases susceptibility, elevating dysbiosis markers (higher F/B, Desulfovibrio). These results suggest SeNPs mitigate oxidative injury by integrating host antioxidant signaling and microbiota-driven metabolic support, highlighting SeNPs as a promising nutritional strategy for preventing intestinal barrier dysfunction.
Dietary supplementation with biogenic Se nanoparticles synthesized by L. casei ATCC 393 prevents oxidative stress-induced intestinal barrier dysfunction in mice by enhancing antioxidant defenses, reducing ROS, preserving mitochondrial structure and function, suppressing NLRP3 inflammasome activation via Nrf2 pathway activation, and promoting a healthier gut microbiota with increased SCFAs. Se deficiency induces a dysbiotic microbiota that heightens susceptibility to oxidative injury, whereas supranutritional SeNPs optimize the microbiota to confer protection, as confirmed by FMT. Future research should elucidate precise microbiota-derived mediators and host pathways linking SeNPs to Nrf2 activation, assess long-term safety and dose–response of SeNPs, and validate translational relevance in human intestinal disease settings.
The study was conducted in mouse models with acute oxidative injury induced by diquat, which may not fully replicate chronic human intestinal diseases. While FMT implicates microbiota involvement, specific microbial species and metabolites causally responsible for protection were not isolated, and functional predictions were inferred (PICRUSt2) rather than directly measured beyond SCFAs. Mechanistic details linking SeNPs, microbiota changes, and Nrf2/NLRP3 signaling require further elucidation. Only two SeNPs supplementation levels were tested against a Se-deficient baseline, and long-term safety and efficacy in diverse conditions were not assessed.
Related Publications
Explore these studies to deepen your understanding of the subject.