Medicine and Health
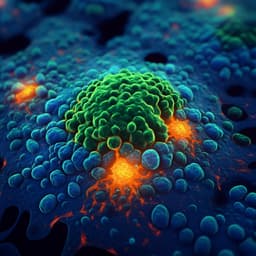
Defective activation and regulation of type I interferon immunity is associated with increasing COVID-19 severity
D. Duffy
This groundbreaking study by Darragh Duffy uncovers the vital role of type I interferons in COVID-19 severity, revealing that diminished IFN-I responses correlate with worsened disease outcomes. With sensitive assays highlighting impaired IFN-I induction in hospitalized patients, the research sheds light on why current IFN-I treatments may falter late in the infection, paving the way for innovative therapeutic strategies.
Playback language: English
Related Publications
Explore these studies to deepen your understanding of the subject.