Medicine and Health
Critical roles of cytokine storm and bacterial infection in patients with COVID-19: therapeutic potential of mesenchymal stem cells
B. Arjmand, S. Alavi-moghadam, et al.
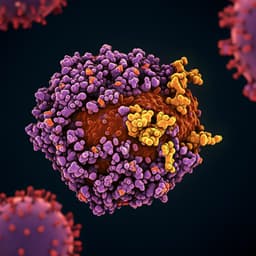
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of COVID-19, produces a wide clinical spectrum from asymptomatic infection to severe pneumonia, ARDS, shock, multi-organ dysfunction, and death. Hyperinflammation and cytokine release syndrome (CRS) and secondary bacterial co-infections are key lethal complications, with gastrointestinal involvement potentially exacerbating hyperinflammation via bacterial translocation. Managing COVID-19 in patients with immune-mediated diseases (e.g., RA) and those on immunosuppressants is challenging. Although secondary bacterial infections occur at an overall low rate, proportions are higher among critical cases, emphasizing rapid diagnosis and timely treatment. Environmental exposures, healthcare contacts, and procedures (e.g., intubation) increase risk of opportunistic secondary infections during isolation, hospitalization, and convalescence. Conventional therapeutics (corticosteroids, antibiotics) are insufficient in many complicated cases, creating a need for new modalities such as regenerative medicine and cell therapy. This review explores COVID-19 immunopathology and pathophysiology, comorbidities such as secondary/co-bacterial infections, and the therapeutic potential of mesenchymal stem cells (MSCs).
Immunopathology and immune responses: The review summarizes innate and adaptive immune responses to SARS-CoV-2. Early viral replication may suppress innate immunity, while later exaggerated responses can culminate in CRS and ARDS. ACE2 facilitates viral entry and its downregulation perturbs RAAS, contributing to organ damage. Innate responses (IFNs, chemokines, recruitment of PMNs, monocytes, NK cells, DCs) and adaptive responses (neutralizing antibodies from B cells, CD8 cytotoxicity, CD4 T-cell help) differ by disease severity. NK cells bridge innate-adaptive immunity but can become exhausted; adoptive NK therapies are proposed.
Key inflammatory signaling pathways: Multiple cascades implicated in COVID-19 hyperinflammation are reviewed, including JAK/STAT (downstream of cytokine receptors and potentially linked to ACE2 hyperactivation), NF-κB (upregulated by viral proteins; central to IL-1, IL-6, TNF production), NLRP3 inflammasome (activated by viral factors leading to IL-1β/IL-18 release and linked to multi-organ involvement), MAPK (ERK, p38, JNK) influencing replication, apoptosis, and inflammation, and Notch signaling (including FURIN-mediated spike processing; cross-talk with cardiovascular complications). Dysregulated RAAS (ACE2/Ang II/AT1R) and ADAM17 sheddase activity contribute to cytokine and receptor shedding and pro-inflammatory signaling.
Bacterial infections in COVID-19: The review details potential for gastrointestinal-mediated bacterial translocation and common bacterial pathogens in viral pneumonia (e.g., Staphylococcus aureus, Streptococcus pneumoniae, Klebsiella pneumoniae, Haemophilus influenzae, Pseudomonas aeruginosa, Serratia marcescens, Listeria monocytogenes) and atypical bacteria (Mycoplasma pneumoniae, Chlamydia pneumoniae, Legionella pneumophila). Co-infection prevalence across studies is generally low overall but higher in severe/critical cases; meta-analyses estimate bacterial infection rates of approximately 5.9–8.1% overall, with higher susceptibility in ICU/ventilated patients. Gram-negative co-infections are frequent in fatal cases. Risk factors include critical illness, immunosuppression, COPD, prolonged hospitalization, invasive devices, mechanical ventilation (risk of VAP), environmental exposure, and potential endotoxemia from gut dysbiosis. Routine broad-spectrum antibiotic prophylaxis is discouraged due to resistance and stewardship concerns.
Therapeutic interventions: Drug therapies target key inflammatory pathways and viral replication (e.g., remdesivir; anti-IL-6R monoclonal antibodies tocilizumab and sarilumab; corticosteroids particularly in ARDS; stewardship-guided antibiotics when indicated). The review compiles pathway-based targets and interventional strategies.
Regenerative medicine and MSCs: MSCs exhibit immunomodulatory, anti-inflammatory, regenerative, and antimicrobial properties. In inflammatory milieus (high TNF and IFN-γ), MSCs adopt an immunosuppressive phenotype via IDO, PGE2, NO, TGF-β, HGF, HO, promoting Tregs and dampening T-cell proliferation. In low-inflammatory contexts, MSCs may secrete chemokines (e.g., MIP-1α, RANTES/CCL5, CXCL9, CXCL10) and enhance immune responses. MSCs preferentially home to the lungs, modulating fibrosis, vascular barrier integrity, and endogenous repair. Antimicrobial effects involve secretion of peptides (LL-37), lipocalin-2 upregulation, and synergy with host immunity and antibiotics. Preclinical ARDS models and multiple clinical trials in COVID-19 have assessed MSCs and MSC-derived extracellular vesicles (EVs), with early safety signals and mixed efficacy endpoints reported. The review contrasts cell-based MSC therapy with cell-free strategies (EVs, conditioned medium), noting advantages of EVs (lower thrombosis risk, storage stability, reduced tumorigenicity/rejection, modifiable cargo) and regulatory considerations. A large table summarizes ongoing and completed MSC/EV clinical trials for COVID-19, including sources (umbilical cord, bone marrow, adipose, dental pulp), dosing, routes (IV, inhalation), phases, and primary outcomes.
- Cytokine storm (CRS) is a major driver of severe COVID-19 and mortality, characterized by elevated IL-6, IL-7, IL-10, GM-CSF, IFN, TNF, and others.
- Multiple inflammatory signaling pathways (JAK/STAT, NF-κB, NLRP3 inflammasome, MAPK, Notch/RAAS cross-talk) underlie hyperinflammation and represent therapeutic targets.
- Bacterial co-infections/secondary infections occur in a minority overall but are more prevalent in severe/critical illness; meta-analyses estimate 5.9–8.1% overall bacterial infection rates, with higher rates in ICU and ventilated patients, and frequent gram-negative involvement.
- Routine empiric broad-spectrum antibiotic use is not supported for all COVID-19 patients; stewardship is essential to limit resistance, reserving antibiotics for clinically suspected/proven bacterial infections (e.g., life-threatening co-bacterial pneumonia) with short courses (e.g., ~5 days) guided by clinical response.
- Risk factors for bacterial infection include critical illness, mechanical ventilation (VAP), immunosuppression, COPD, prolonged hospitalization, invasive devices, and potential gut-derived endotoxemia.
- Mesenchymal stem cells (MSCs) can attenuate hyperinflammation via paracrine factors (IDO, PGE2, NO, TGF-β, HGF, HO), promote Tregs, modulate macrophage polarization, support endothelial/epithelial repair, and potentially restore barrier integrity in lungs.
- MSCs exhibit antimicrobial actions (e.g., LL-37, lipocalin-2) and can enhance bacterial clearance and survival in preclinical models; they may synergize with antibiotics and innate immunity.
- Clinical studies/trials of MSCs and MSC-derived EVs in COVID-19 show acceptable safety profiles and variable efficacy signals (e.g., oxygenation indices, ventilator withdrawal, cytokine modulation), warranting further rigorous trials and standardization.
- Cell-free MSC-derived products (exosomes/EVs, secretome) offer practical advantages (safety, storage, modifiable cargo) and are under active investigation (including inhaled formulations).
This narrative review integrates immunopathology of COVID-19 with the clinical problem of bacterial co-infections to justify host-directed therapies that can modulate excessive inflammation while supporting antimicrobial defense. By detailing the contribution of JAK/STAT, NF-κB, NLRP3, MAPK, and Notch pathways to CRS, the review highlights rational drug targets (e.g., IL-6R blockade, JAK inhibitors) and underscores limitations of broad antibiotic use. It argues that MSC-based therapies, through multi-modal immunomodulation, tissue repair, and antimicrobial peptide secretion, uniquely address both arms of the problem—attenuating cytokine-driven damage and potentially reducing susceptibility to and severity of secondary bacterial infections. Early clinical experiences suggest safety and feasibility, but heterogeneous protocols, sources, and endpoints necessitate standardized, well-controlled studies to define efficacy, dosing, timing, and patient selection. In the broader field, MSCs and their cell-free derivatives may complement antiviral and anti-inflammatory regimens, especially in severe COVID-19 with ARDS and co-infections.
Effective management of severe COVID-19 requires controlling hyperinflammation and mitigating bacterial co-infections. Mesenchymal stem cells and their derivatives emerge as promising adjuncts due to their immunomodulatory, regenerative, and antimicrobial properties. Future work should: (1) standardize MSC sourcing, characterization, dosing, and administration; (2) elucidate mechanisms across inflammatory pathways and host defense; (3) develop precision approaches by matching MSC source/phenotype to patient profiles; (4) advance cell-free strategies (EVs/secretome) and delivery systems (including inhalation) to improve safety and scalability; and (5) conduct high-quality randomized controlled trials with harmonized endpoints. Coordinated regulatory guidance and international consensus will be essential to translate MSC-based therapies into evidence-based care for COVID-19 and related hyperinflammatory syndromes.
As a narrative review, no systematic search strategy or bias assessment is described. Evidence on bacterial co-infections in COVID-19 remains heterogeneous, with limited high-quality prospective data and variable definitions across studies. Many MSC studies are small, single-center, or early phase with differing cell sources, manufacturing protocols, doses, and outcomes, limiting comparability and generalizability. Rapid pandemic timelines shifted focus from preclinical to clinical studies, leaving gaps in mechanistic and translational data. Potential risks of cell-based therapy (e.g., pro-tumor effects, thrombosis) and regulatory variability necessitate careful evaluation. Further rigorous, standardized trials and mechanistic studies are required.
Related Publications
Explore these studies to deepen your understanding of the subject.