Medicine and Health
Combination of pre-adapted bacteriophage therapy and antibiotics for treatment of fracture-related infection due to pandrug-resistant *Klebsiella pneumoniae*
A. Eskenazi, C. Lood, et al.
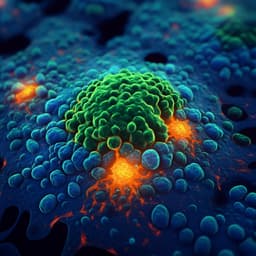
A groundbreaking study reveals the successful treatment of a 30-year-old bombing victim suffering from a pandrug-resistant *Klebsiella pneumoniae* infection. Using a novel combination of pre-adapted bacteriophage therapy alongside antibiotics, this research conducted by authors from various esteemed institutions demonstrates significant clinical and microbiological improvements. Discover how this innovative approach is reshaping the fight against antibiotic resistance!
Related Publications
Explore these studies to deepen your understanding of the subject.