Medicine and Health
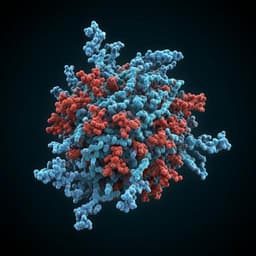
Antibodies targeting the Crimean-Congo Hemorrhagic Fever Virus nucleoprotein protect via TRIM21
S. S. Leventhal, T. Bisom, et al.
Discover groundbreaking research on the Crimean-Congo Hemorrhagic Fever Virus, revealing how a self-replicating RNA vaccine induces neutralizing antibodies and protective immunity through TRIM21. This exciting study by Shanna S Leventhal and colleagues sheds new light on the mechanisms of protection against this lethal virus.
~3 min • Beginner • English
Introduction
Crimean-Congo hemorrhagic fever (CCHF) is an emerging, highly pathogenic tick-borne disease caused by CCHFV with expanding geographic risk driven by vector spread and climate change. Human infection occurs via tick bites, exposure to infected animal blood, and nosocomial transmission. Disease begins with non-specific febrile symptoms and can rapidly progress to severe hemorrhagic manifestations with reported case fatality rates ranging from 5% to 70%, influenced by surveillance and reporting infrastructure. No widely approved vaccines or effective therapeutics are currently available, prompting WHO to list CCHFV as a priority pathogen. CCHFV, a nairovirus with a tri-segmented negative-sense RNA genome (S, M, L), encodes the nucleoprotein (NP) on the S segment, which encapsidates viral RNA, supports replication, and modulates host responses. While glycoprotein (GP)-targeting neutralizing antibodies can be protective in animal models, non-neutralizing antibodies may also contribute. Recent vaccine studies demonstrated that responses to NP and NSs can confer protection, suggesting NP is a viable vaccine antigen. This study investigates whether vaccine-elicited anti-NP antibodies protect against CCHFV, defines the effector mechanisms involved, and evaluates the role of TRIM21 in antibody-mediated protection.
Literature Review
Prior work in CCHFV models indicated that glycoprotein-directed neutralizing antibodies contribute to protection, though non-neutralizing antibodies can also be protective in some contexts. DNA- and RNA-based vaccines expressing NP have protected nonhuman primates and mice, implicating NP-specific immunity in disease control. TRIM21, a cytosolic Fc receptor that binds antibody-coated antigens and targets them for proteasomal degradation while stimulating innate sensing pathways, has been shown to mediate intracellular neutralization and enhance antigen presentation in other viral systems (e.g., LCMV NP, adenovirus, rotavirus). Human studies associate the appearance of anti-NP IgM/IgG with viral clearance in CCHF, whereas fatal cases may lack NP-specific responses despite GP-specific antibodies. These observations motivated testing whether NP-directed antibodies can protect via TRIM21 in vivo and in vitro.
Methodology
- Vaccine and passive transfer: A self-replicating alphavirus-based RNA (repRNA) vaccine expressing CCHFV NP (repNP) was administered intramuscularly to C57BL/6 background mice. For passive transfer, pooled sera from repNP- or sham-vaccinated mice were collected and administered (typically 200 μL; an additional study used 400 μL given 6 h pre-challenge). In some challenges, type I IFN signaling was transiently suppressed with MAR1-5A3 anti-IFNAR1 antibody.
- Mouse models and depletions: Vaccine efficacy was tested in WT mice and those deficient in activating Fcγ receptors (FcγR−/−), complement component C3 (C3−/−), or TRIM21 (TRIM21−/−). NK cells were depleted in WT mice using anti-NK1.1 on a defined schedule. T cell involvement was probed via CD4/CD8 antibody-mediated depletion and in CD8−/− mice. Immune responses were profiled by whole-virion ELISA (isotypes/subclasses) and IFNγ ELISpot for NP-specific T cells.
- Virus challenge and readouts: Mice were challenged intravenously with a lethal dose of CCHFV strain UG3010; a mouse-adapted CCHFV (MA-CCHFV) was used for certain in vitro assays. Clinical disease, weight, and survival were monitored up to 14 days post-infection. On day 5 post-infection, viral loads in blood, liver, and spleen were quantified by TCID50 and qRT-PCR; tissues underwent histopathology and immunohistochemistry.
- NP surface detection: CCHFV-infected mouse L929 fibroblasts and human A549 epithelial cells were stained for NP by immunofluorescence under permeabilized and non-permeabilized conditions to assess surface expression.
- Intracellular neutralization (EDNA/ADIN): L929 cells (WT or TRIM21−/−) were electroporated with mouse, macaque, or human sera (NP-immune vs controls) to deliver antibodies intracellularly, then infected with CCHFV or MA-CCHFV. Supernatant virus at 72 h post-infection was measured by TCID50 to derive inhibitory concentrations (IC50). Electroporation efficiency was validated by uptake of fluorescently labeled antibodies by flow cytometry.
- Nonhuman primate and human sera: Sera from repNP-vaccinated cynomolgus macaques (pre-immune and post-boost) and from CCHFV-exposed humans (ELISA-confirmed) were tested for ELISA reactivity and EDNA-mediated inhibition in WT vs TRIM21−/− cells.
- Statistics: Analyses were performed in GraphPad Prism; survival and viral load comparisons used appropriate tests as indicated (e.g., one-way ANOVA).
Key Findings
- Passive transfer of anti-NP antibodies protects: Transfer of 200 μL repNP-immune sera to naive mice delayed disease and improved survival from 0% in sham to approximately 40–50%. Increasing the dose/timing (400 μL administered 6 h before challenge) raised survival to 75% (9/12) in WT mice.
- Fcγ receptors, complement, and NK cells not required: repNP-vaccinated FcγR−/− mice, C3−/− mice, and WT mice depleted of NK cells remained protected. Complement deficiency modestly reduced protection but differences were marginal.
- TRIM21 is essential for vaccine-mediated protection: TRIM21−/− mice vaccinated with repNP mounted robust NP-specific antibody responses comparable to WT but failed to gain protection, exhibiting survival and viral loads similar to sham and significant liver/splenic pathology. Thus, TRIM21 is required for protection by NP vaccination in vivo.
- TRIM21 is required for passive serum protection: Passive transfer of NP-immune sera protected WT mice (75% survival) but provided no protection in TRIM21−/− recipients.
- Protection is independent of T cells: repNP vaccination protected mice depleted of CD4 and CD8 T cells and protected CD8−/− mice, and NP-specific T cell responses after infection were similar in WT vs TRIM21−/− groups.
- Intracellular neutralization demonstrated and enhanced by TRIM21: In EDNA assays, intracellular delivery of NP-immune sera (mouse and macaque) inhibited CCHFV replication in L929 cells; inhibition was significantly potentiated by TRIM21 (e.g., ~3-fold stronger inhibition in WT vs TRIM21−/− for macaque sera). Human convalescent sera also inhibited replication, enhanced by TRIM21.
- NP detection on infected cell surface is cell type dependent: NP was not detected on the surface of unpermeabilized L929 cells but was detectable on A549 cells, suggesting limited roles for classical Fc effector mechanisms in some cell types and supporting a cytosolic TRIM21 mechanism.
- Histopathology: WT repNP-vaccinated mice showed normal liver histology, whereas sham and TRIM21−/− repNP-vaccinated mice showed multifocal hepatic necrosis and viral antigen by IHC.
- Survival statistics: Reported significant survival benefits for WT mice receiving NP-immune sera (one-way ANOVA; examples include P = 0.001 and P = 0.0008 for survival comparisons in figures).
Discussion
The study demonstrates that NP-specific antibodies can protect against lethal CCHFV infection through a TRIM21-dependent intracellular mechanism rather than through classical Fcγ receptor-mediated cytotoxicity or complement activation. TRIM21 likely binds the Fc of NP-bound antibodies delivered into the cytosol, targeting NP for proteasomal degradation and potentiating innate sensing, thereby restricting viral replication. The requirement for TRIM21 in both active vaccination and passive transfer establishes intracellular antibody immunity as a key antiviral pathway against an enveloped virus. The independence from T cells for protection in this model underscores the sufficiency of humoral, TRIM21-mediated mechanisms for survival. EDNA experiments corroborate in vivo findings by showing intracellular neutralization enhanced by TRIM21 across mouse, primate, and human sera. Detection of NP on the surface of some infected cells suggests potential heterogeneity in antigen availability for extracellular mechanisms, but the dominant protective route observed was intracellular and TRIM21-dependent. These findings have broad implications for vaccine design targeting internal viral antigens and for antibody-based therapeutics that leverage TRIM21.
Conclusion
NP-targeted vaccination elicits antibodies that protect against CCHFV via TRIM21 in vivo. Passive transfer of NP-immune sera confers significant protection in WT but not TRIM21−/− mice, and vaccine-mediated protection does not require Fcγ receptors, complement, NK cells, or T cells. Intracellular neutralization assays confirm that TRIM21 enhances antibody-mediated inhibition of CCHFV replication. These results expand understanding of TRIM21’s antiviral role against enveloped viruses and support NP as a protective vaccine antigen. Future work should define how NP–antibody complexes access the cytosol during infection, delineate the role of proteasomal degradation and innate sensing pathways downstream of TRIM21, and evaluate optimized monoclonal antibody therapeutics and dosing/therapeutic windows in preclinical models and ultimately in humans.
Limitations
- Mechanism of cytosolic access is unresolved: How NP–antibody complexes reach the cytoplasm to engage TRIM21 in vivo remains unclear for an enveloped virus; possibilities include endosomal disruption, extracellular NP release, or cell-type specific antigen exposure.
- Partial efficacy of passive transfer: Protection by sera transfer was incomplete at standard dosing, improved with higher volume and timing, suggesting dose and kinetics constraints and a need to define therapeutic windows.
- Species and model constraints: Most experiments were in mice, including IFNAR blockade contexts, which may not fully reproduce human disease; NP surface presentation was cell-type dependent (A549 vs L929), limiting generalizability of extracellular mechanisms.
- Human sera specificity: Inhibition observed with human sera may involve antibodies to other viral proteins; contributions cannot be fully excluded.
- Complement role nuance: While not required for protection, complement may contribute to optimal vaccine-induced responses; precise contributions were not fully delineated.
- Post-exposure treatment: A previously reported anti-NP monoclonal showed limited efficacy post-infection, highlighting potential constraints for therapeutic use that require further optimization.
Related Publications
Explore these studies to deepen your understanding of the subject.