Medicine and Health
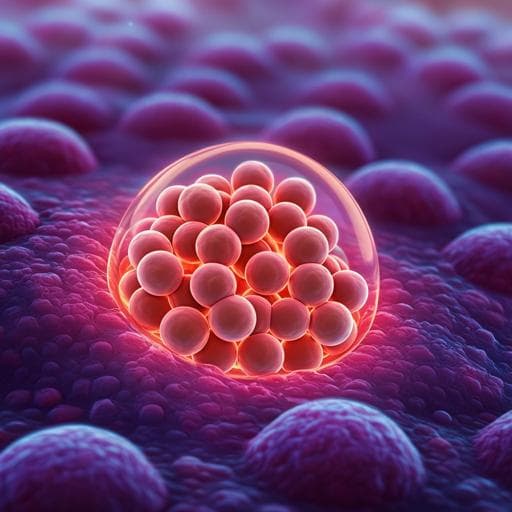
An injectable photopolymerized hydrogel with antimicrobial and biocompatible properties for infected skin regeneration
A. Sun, X. He, et al.
Discover an innovative injectable hydrogel designed to combat infected wounds! This groundbreaking research by Ao Sun, Xinye He, Lang Li, Tao Li, Qinya Liu, Xinli Zhou, Xiao Ji, Wei Li, and Zhiyong Qian showcases a biocompatible solution with impressive antimicrobial properties, capable of promoting healing in Staphylococcus aureus-infected models.
Related Publications
Explore these studies to deepen your understanding of the subject.