Medicine and Health
Advancements in clinical aspects of targeted therapy and immunotherapy in breast cancer
F. Ye, S. Dewanjee, et al.
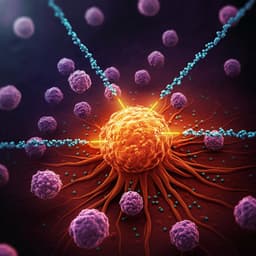
Despite ongoing medical advances, breast cancer remains the second most widespread and fatal malignancy in females. During the past four decades, breast cancer incidences have risen alarmingly. In 2020, there were approximately 2.3 million new cases of breast cancer worldwide, and there were also roughly 685,000 deaths from this illness, with notable geographic variations between various countries and regions. Notably, high-economic nations represent a greater percentage of breast cancer fatalities. By 2040, it has been anticipated that there will be more than 3 million new instances of breast cancer each year with more than 1 million annual deaths. There are several different forms of breast carcinoma. It has been found that steroid hormone receptors (HRs) are significant prognostic factors for breast cancer. Breast cancer cells with HRs expressing estrogen (ER), progesterone (PR), or both are referred to as ER-positive (ER+), PR-positive (PR+), or ER/PR positive (ER+/PR+) breast cancers, respectively. Most breast carcinomas are ER+ and of those, more than half are both ER+/PR+; while, only about 2% are solely PR+. Triple-negative breast cancer (TNBC) refers to the cancerous cells lacking ER and PR as well as making too little or no expression of human epidermal growth receptor 2 (HER2). About 10-15% of all breast carcinomas are TNBC. In recent years immunogenic prospects of breast tumor have been revealed. The discovery of tumor-infiltrating lymphocytes (TILs) within breast cancers demonstrated the immunogenic character of breast cancer. Analysis of breast tumor samples revealed that individuals with HER2-positive (HER2+) and TNBC had a greater number of TILs than those of HR-positive (HR+) subtypes.
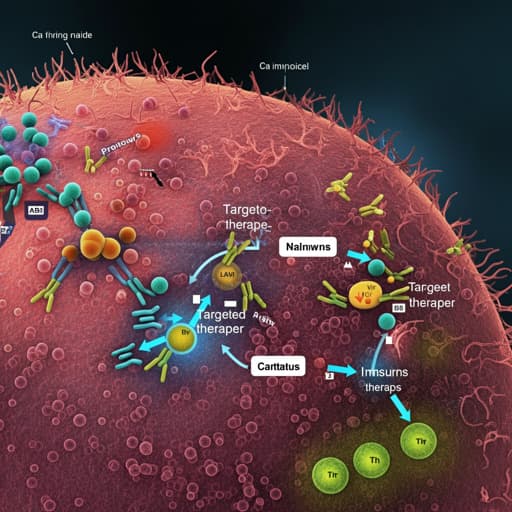
After decades of endocrine and other therapies, an improved understanding of immune evasion by cancerous cells and the creation of specific immune checkpoint antagonists have unveiled new therapeutic options. Immunotherapy involves the enhancement of host immunity and admits cancer as a foreign antigen, which leads to the destruction of cancer cells. However, some adverse events have been advocated in the patients who received immunotherapies, which include fatigue, nausea, vomiting, dizziness, and pruritus. Enterocolitis, endocrinopathies, liver anomalies, and uveitis are some additional immune-related side effects that can result from using immunotherapeutics like ipilimumab. Immune checkpoint blockers are being used in conjunction with chemotherapy, targeted therapy, and radiation therapy under intense examination due to the low efficacy of previous immunotherapeutic drugs in treating many kinds of breast carcinoma. On the other hand, breast cancer-targeted therapies use substances or drugs to inhibit disease progression by obstructing certain components essential for cancer cell survival, proliferation, and migration, as well as for angiogenesis. Poly (ADP-ribose) polymerase (PARP), cyclin-dependent kinase (CDK) 4 and 6 (CDK4/6), Ak strain transforming (AKT), and fibroblast growth factor receptor (FGFR) are well-established therapeutic targets that have been the main focus of drug development for the treatment of breast cancer. Patients under targeted therapy also deal with some common side effects such as nausea, vomiting, diarrhea, tiredness, and rashes. Thus, adequate attention must be given to address the toxicity concerns of both the targeted and immune therapies. This review gives a concise overview of the different targeted and immunotherapies used to treat breast cancer and the effectiveness and safety of these approaches in clinical settings.
This review synthesizes clinical advancements in targeted therapy (PARP, CDK4/6, AKT, angiogenesis, and FGFR inhibitors) and immunotherapy (immune checkpoint blockade, therapeutic vaccines, and adoptive cell therapy) for breast cancer. It details mechanistic rationales (e.g., PRLR–EGFR/HER2 crosstalk; PI3K/AKT/mTOR; cell-cycle control via CDK4/6; angiogenesis via VEGF/VEGFR; FGF/FGFR signaling), summarizes key phase I–III trials, FDA approvals, efficacy signals, and safety profiles across subtypes (HR+/HER2−, HER2+, TNBC). Evidence indicates robust benefits for PARP inhibitors (olaparib, talazoparib) in gBRCA-mutated HER2− disease; CDK4/6 inhibitors (palbociclib, ribociclib, abemaciclib) combined with endocrine therapy in HR+/HER2− disease; mixed outcomes for AKT inhibitors (capivasertib, ipatasertib); limited overall survival gains with anti-angiogenics; and ongoing development of FGFR inhibitors. For immunotherapy, PD-1/PD-L1 inhibitors (pembrolizumab, atezolizumab, durvalumab, avelumab, nivolumab) show the greatest promise in TNBC, particularly PD-L1-positive tumors and in combination with chemotherapy. CTLA-4 blockade (ipilimumab, tremelimumab) has niche activity, often in combination. Therapeutic vaccines targeting HER2 (E75/nelipepimut-S, GP2, AE37), MUC1, MAM-A, hTERT, and carbohydrate antigens report immunogenicity with variable clinical efficacy. Adoptive strategies (TILs, CAR-T, TCR-engineered cells, dendritic cells, NK cells) are in early-phase trials with encouraging yet heterogeneous results and safety considerations.
- Targeted therapy
- PARP inhibitors: Olaparib improved progression-free survival by 2.8 months versus standard therapy in gBRCA-mutated, HER2− metastatic breast cancer (OlympiAD, NCT02000622), with reported reduction in death risk; combination regimens (e.g., with carboplatin, eribulin, durvalumab) show activity with hematologic toxicities (e.g., neutropenia). Adjuvant olaparib prolonged invasive disease-free survival in high-risk HER2− early breast cancer with gBRCA mutations (NCT02032823). Talazoparib demonstrated significant response rates (50% in phase I; superior PFS over chemotherapy in EMBRACA) with manageable hematologic AEs. Rucaparib and niraparib showed limited or mixed efficacy signals in breast cancer; BRAVO (niraparib) was halted due to assessment discrepancies.
- CDK4/6 inhibitors: Palbociclib plus letrozole improved PFS in ER+/HER2− advanced disease (PALOMA-1); palbociclib plus fulvestrant improved survival trends (PALOMA-3). Ribociclib plus letrozole significantly prolonged PFS (25.3 vs 16.0 months; NCT01958021) and benefited premenopausal women (MONALEESA-7). Abemaciclib showed efficacy as monotherapy and with fulvestrant or aromatase inhibitors (MONARCH-2/3), with diarrhea and hematologic AEs manageable; rare lung inflammation warnings apply to the class.
- AKT inhibitors: Capivasertib demonstrated tumor shrinkage in PIK3CA-mutant tumors; with fulvestrant, improved PFS in ER+ metastatic disease (FAKTION). Benefit in TNBC with paclitaxel (PAKT) was observed, while other studies showed mixed results; on-target pathway suppression was confirmed in neoadjuvant biomarker trials (STAKT). Ipatasertib improved PFS in metastatic TNBC with paclitaxel (LOTUS) but failed to improve outcomes in HR+/HER2− cohort (IPATunity130 B) and had mixed neoadjuvant results (FAIRLANE).
- Angiogenesis inhibitors: Bevacizumab combinations improved response rates and PFS in some trials (e.g., E2100) but did not consistently improve overall survival; subsequent trials (AVADO, RIBBON) showed less benefit. Ramucirumab and several VEGFR TKIs (cediranib, vandetanib, axitinib, pazopanib, sorafenib, sunitinib) produced mixed or limited efficacy and/or increased toxicity.
- FGFR inhibitors: Non-selective TKIs (dovitinib, lucitanib, lenvatinib) and selective FGFR inhibitors (AZD4547, infigratinib, erdafitinib, Debio-1347, TAS-120) are under investigation; early studies show potential activity in FGFR-amplified subsets, but conclusive efficacy in breast cancer remains to be established.
- Immunotherapy
- PD-1/PD-L1 inhibitors: Pembrolizumab monotherapy showed activity in PD-L1+ metastatic TNBC (KEYNOTE-012/086) but did not improve OS versus chemotherapy in pretreated TNBC overall (KEYNOTE-119); addition to chemotherapy improved PFS in untreated metastatic TNBC (KEYNOTE-355). Atezolizumab plus nab-paclitaxel improved PFS in PD-L1+ metastatic TNBC (IMpassion130), though OS benefit was limited; IMpassion131 with paclitaxel was negative. Durvalumab combinations (e.g., with chemotherapy or olaparib) improved pathologic complete response or showed maintenance OS signals in subsets; benefit enriched in PD-L1+ patients. Nivolumab demonstrated responses with induction therapies in TNBC (TONIC). Avelumab had modest efficacy, with higher responses in PD-L1+ immune cell–rich TNBC.
- CTLA-4 inhibitors: Tremelimumab and ipilimumab showed limited single-agent activity; combinations (with durvalumab or nivolumab, chemotherapy, or radiotherapy) produced responses in select subtypes (e.g., metaplastic TNBC) but with notable immune-related AEs.
- Vaccines: HER2 peptide/protein/DNA vaccines (E75/nelipepimut-S, GP2, AE37, recombinant HER2 protein) elicited immune responses and signals of reduced recurrence in subgroups, but phase III results have been mixed or negative overall. Non-HER2 vaccines (MUC1, PANVAC, MAM-A, hTERT, carbohydrate antigens like STn and Globo H) induced immunogenicity with variable clinical impact; ongoing phase III (e.g., Globo H–targeted) aims to clarify benefit in high-risk TNBC.
- Adoptive cell therapy: TIL therapy and engineered TCR/CAR-T approaches targeting antigens such as HER2, MUC1, c-Met, mesothelin, ROR1, and NKG2D ligands are in early clinical development. Case reports and early trials show durable regressions in select patients, but challenges include on-target/off-tumor toxicity and variable efficacy; strategies targeting tumor-specific glycoforms may improve selectivity and safety.
- Cross-cutting insights: Biomarker-driven selection (e.g., gBRCA, PD-L1, PIK3CA/PTEN/AKT alterations, FGFR amplifications) is crucial. Toxicities (hematologic for PARP/CDK4/6; diarrhea and rash for AKT inhibitors; immune-related AEs for checkpoint inhibitors) require proactive management. TNBC benefits most from immunotherapy, particularly PD-L1+ disease, but many patients remain non-responders.
The review addresses the central challenge of breast cancer heterogeneity by mapping therapeutic strategies to molecular subtypes and immune context. Targeted therapies effectively exploit defined vulnerabilities (e.g., DNA repair defects in gBRCA-mutated tumors; cell-cycle dependence in HR+/HER2− disease), while immunotherapy expands options for TNBC, a historically chemotherapy-only subtype. Evidence supports combination approaches—checkpoint inhibitors with chemotherapy or PARP inhibitors; endocrine therapy with CDK4/6 inhibitors; and rational pairings within PI3K/AKT/mTOR signaling—to enhance efficacy and overcome resistance. However, benefits are often confined to biomarker-enriched populations (e.g., PD-L1 positivity, pathway mutations), underscoring the need for comprehensive molecular and immune profiling. Safety profiles vary across modalities and can be limiting; thus, individualized risk–benefit assessment and toxicity monitoring are essential. The review emphasizes overcoming primary and acquired resistance, optimizing biomarkers (PD-L1, TMB, TILs, HLA-I), and refining the tumor microenvironment to improve immunotherapeutic responsiveness, particularly in TNBC.
The recent advancements in targeted therapy offer specific and effective options by inhibiting molecules essential for tumor growth and survival. Several agents have gained FDA approvals as monotherapy or in combinations for defined breast cancer subtypes, while many others are in clinical trials. Nonetheless, drug resistance and limited efficacy in TNBC remain major challenges. Immunotherapies, especially immune-checkpoint inhibitors combined with chemotherapy, have emerged as promising treatments for TNBC, with some regimens approved and many under investigation. Given the profound heterogeneity of breast cancer, achieving optimal outcomes with targeted or immune therapies requires a deep understanding of the molecular, genetic, and immunological landscape of tumors and their microenvironments. Discovering and validating precise biomarkers to guide personalized treatment is urgently needed to determine accurate therapeutic regimens and improve patient outcomes.
As a narrative review, no primary experimental methodology is presented. Reported clinical outcomes are drawn from heterogeneous trials with varying designs, endpoints, biomarker assays, and patient populations, limiting cross-trial comparability. Many promising findings are from early-phase or subset analyses and require confirmation in phase III studies. Efficacy of several approaches (e.g., angiogenesis and FGFR inhibitors, vaccines, adoptive cell therapies) remains inconsistent or preliminary. Benefits of immunotherapy are often restricted to PD-L1–positive tumors, leaving many patients without clear benefit. Toxicities from targeted and immune therapies (hematologic, gastrointestinal, immune-related adverse events, rare pulmonary toxicity) may limit generalizability and necessitate careful monitoring. TNBC still lacks broadly effective targeted options beyond immunotherapy in selected patients.
Related Publications
Explore these studies to deepen your understanding of the subject.