Medicine and Health
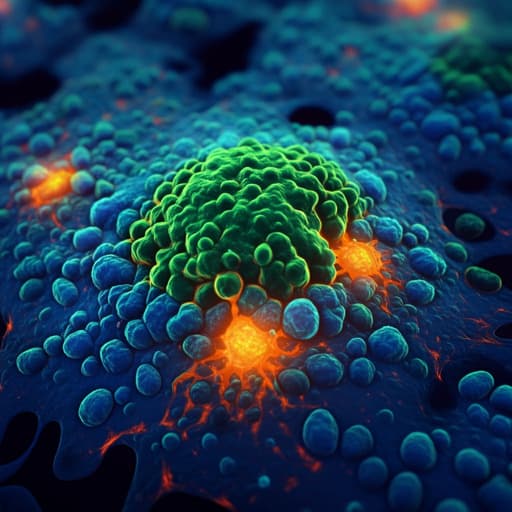
A type I interferon footprint in pre-operative biopsies is an independent biomarker that in combination with CD8+ T cell quantification can improve the prediction of response to neoadjuvant treatment of rectal adenocarcinoma
A. Rezapour, D. Rydbeck, et al.
This groundbreaking study reveals that predicting the response to neoadjuvant treatment in rectal cancer could significantly benefit from the application of multiplex immunofluorescence. By focusing on TILs and type I interferon response, researchers including Azar Rezapour and Daniel Rydbeck provide insights that can help tailor treatments and improve patient outcomes.
Related Publications
Explore these studies to deepen your understanding of the subject.







