Medicine and Health
A single dose of recombinant VSV-ΔG-spike vaccine provides protection against SARS-CoV-2 challenge
Y. Yahalom-ronen, H. Tamir, et al.
SARS-CoV-2, the causative agent of COVID-19, uses the spike (S) glycoprotein to bind ACE2 and enter host cells, making S the primary target for neutralizing antibodies. There is an urgent need for safe, effective, and scalable vaccines. Recombinant vesicular stomatitis virus (rVSV) is an attractive vaccine platform due to high titers in culture, strong immunogenicity, attenuation upon deletion of VSV-G, sensitivity to interferon, and low pre-existing immunity in humans. The study aimed to develop and evaluate an rVSV-based vaccine in which VSV-G is replaced with the SARS-CoV-2 S protein (rVSV-ΔG-spike), test its antigenic authenticity versus SARS-CoV-2, and assess safety, immunogenicity, and protective efficacy in a golden Syrian hamster model of COVID-19.
Prior work established rVSV as a versatile vaccine vector (e.g., rVSV-EBOV), with clinical safety and efficacy demonstrated for Ebola virus vaccines and FDA approval (ERVEBO). Structural and functional studies of SARS-CoV-2 S highlight the importance of the S1/S2 furin cleavage site for entry and pathogenesis, and prior VSV pseudotyping studies showed that cytoplasmic tail truncations of SARS-CoV spikes can enhance incorporation and titers. Small animal models, notably golden Syrian hamsters, reliably recapitulate SARS-CoV-2 pathogenesis with peak viral loads around 3 days post infection in respiratory tissues. These data underpin the rationale for an rVSV-ΔG-spike vaccine and for evaluating it in hamsters.
Vaccine design and rescue: The open reading frame of VSV-G in a full-length VSV cDNA (pVSV-FL+(2)) was replaced with a human codon-optimized full-length SARS-CoV-2 spike (Sino Biological). BHK-21 cells were infected with MVA-T7 and cotransfected with the rVSV-ΔG-spike plasmid and accessory plasmids encoding VSV-N, P, L, and G under T7 control. To support initial entry, VSV-G was transiently supplied via PCAGGS-VSV-G. Supernatant was clarified and filtered twice (0.22 µm) to eliminate MVA-T7 and used to infect cells to generate passage 1. Sequential passaging (≥14 passages) was performed on Vero E6 cells to eliminate VSV-G carryover and adapt the virus. Characterization: qRT-PCR across passages quantified VSV-N, residual VSV-G, and SARS-CoV-2 S; plaque assays measured titers and plaque morphology. Immunofluorescence of infected Vero E6 cells used anti–SARS-CoV-2 antibodies and DAPI; transmission electron microscopy (TEM) with negative staining and RBD-directed immunogold labeling evaluated virion morphology and spike decoration, with spike length measurements. Viral genome sequencing at key passages identified adaptive mutations. Antigenicity and neutralization: Antigenic similarity to SARS-CoV-2 was assessed by staining infected cells with COVID-19 convalescent human sera. Neutralizing capacity was quantified by plaque reduction neutralization tests (PRNT) to determine NT50 against both rVSV-ΔG-spike and authentic SARS-CoV-2; correlation was analyzed by Spearman’s test. Hamster model and vaccination: Golden Syrian hamsters were intranasally infected with SARS-CoV-2 at 5×10^4, 5×10^5, or 5×10^6 pfu to establish dose–response in body weight loss and lung pathology; 5×10^6 pfu was selected for challenge. For vaccination, hamsters received a single intramuscular dose of rVSV-ΔG-spike at 10^4–10^8 pfu; safety was monitored by weight and clinical observations. Neutralizing antibody responses post-vaccination were measured by PRNT; sera binding was shown by immunofluorescence of SARS-CoV-2–infected cells. Approximately 25 days after vaccination, hamsters were challenged intranasally with 5×10^6 pfu SARS-CoV-2 and monitored for 12 days. Viral load and pathology: At defined time points (3 and/or 5 dpi), lungs and nasal turbinates were harvested for infectious viral titration by plaque assay (limits of detection: lungs 75 pfu/lung; turbinates 50 pfu/sample). Lungs underwent histopathological evaluation (H&E) and SARS-CoV-2 antigen detection by DAB immunohistochemistry with digital quantification of positive cells. Lung injury was scored using American Thoracic Society criteria (neutrophils in alveoli/interstitium, fibrin, cellular debris, septal thickening). Tissue/air space ratio was quantified via ImageJ particle analysis from standardized x20 images. Isotype profiling in mice: Due to limited hamster reagents, C57BL/6J mice received 10^7 pfu rVSV-ΔG-spike i.m.; sera at day 14 were tested by PRNT (NT50) and ELISA against stabilized S2P antigen for total IgG, IgG2c (Th1 surrogate), and IgG1 (Th2 surrogate). Statistics: Body weight over time analyzed by unpaired t-tests with Holm–Sidak correction; neutralization correlations by Spearman’s r; viral load comparisons by Kruskal–Wallis or Mann–Whitney tests; isotype comparisons by Kruskal–Wallis; histology by one-way ANOVA with Tukey’s post hoc test.
- Successful rescue and adaptation: Sequential passaging eliminated VSV-G by passage 10 and increased titers to 3×10^7 pfu/ml at passage 13; plaque formation emerged at later passages as syncytia diminished.
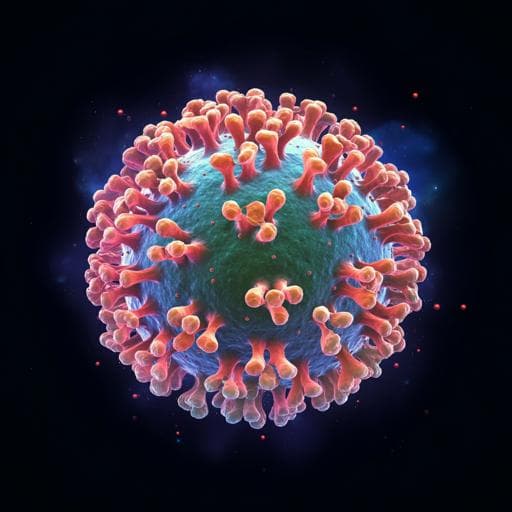
- Structural/antigenic authenticity: TEM showed bullet-shaped virions decorated with spike structures (12–20 nm) consistent with SARS-CoV-2 S; immunogold labeling with anti-RBD confirmed spike presence. In infected cells, human convalescent sera recognized S in both rVSV-ΔG-spike and SARS-CoV-2 infections. Neutralization NT50 values against rVSV-ΔG-spike strongly correlated with those against authentic SARS-CoV-2 (Spearman r=0.944, p<0.0001; n=12 sera).
- Adaptive spike mutations: Three mutations arose by passage 9: P507P (synonymous), R685G altering the multibasic S1/S2 furin motif (RRAR→RRAG), and C1250* introducing a stop codon truncating 24 amino acids from the cytoplasmic tail; these became dominant with increased titers.
- Hamster model establishment: Intranasal infection caused dose-dependent weight loss up to ~17% at 5×10^6 pfu and characteristic lung pathology; 5×10^6 pfu was used for challenge.
- Safety and immunogenicity: Single-dose i.m. vaccination (10^4–10^8 pfu) was well-tolerated with continued weight gain pre-challenge. All doses induced neutralizing antibodies in a dose-dependent manner.
- Protection from disease: After challenge (5×10^6 pfu), unvaccinated hamsters showed gradual weight loss to 5 dpi; vaccinated groups exhibited only mild, transient loss followed by recovery, with significant improvements at 4–7 dpi for most doses (10^4 significant at 6–7 dpi).
- Viral load reduction: At 5 dpi, unvaccinated lungs had mean 1.3×10^5 pfu/lung (n=7), whereas all vaccinated groups (10^4–10^8 pfu; n=3/group) were below LOD (75 pfu/lung; p=0.0012). At 3 dpi (10^6 pfu vaccine): lungs decreased from 5.6×10^6 to 7.3×10^3 pfu/lung (n=4 each; p=0.0286); nasal turbinates decreased from 1.9×10^5 to 2.8×10^2 pfu/sample (n=4 each; p=0.0286), i.e., ~3-log reductions.
- Histopathological protection: Vaccination markedly reduced lung injury scores at 3 and 7 dpi, decreased SARS-CoV-2 DAB-positive cells from 20.16% (3 dpi) and 7.87% (7 dpi) in infected to 2.0% and 1.05% in vaccinated+infected lungs, and restored tissue/air space ratios toward naive levels.
- Th1-biased response in mice: Mice vaccinated i.m. (10^7 pfu) developed high neutralization titers (NT50 range 825–2548) and significantly higher IgG2c vs IgG1 against S2P, indicating a Th1-skewed humoral response.
The study demonstrates that replacing VSV-G with SARS-CoV-2 S yields a replication-competent rVSV-ΔG-spike vaccine that robustly expresses spike on virions and infected cells, preserves antigenicity relative to authentic SARS-CoV-2, and elicits neutralizing antibodies. In hamsters, a single intramuscular dose provided strong protection against high-dose intranasal challenge, as evidenced by minimal weight loss, profound reductions or clearance of infectious virus from lungs and nasal turbinates, and significantly mitigated lung pathology. The strong correlation between neutralization of rVSV-ΔG-spike and SARS-CoV-2 supports the vaccine’s antigenic authenticity and its utility for immunogenicity assessments. Adaptive mutations (R685G at the S1/S2 furin site and a 24-aa cytoplasmic tail truncation) likely facilitated efficient replication in Vero E6 cells, improved assembly/incorporation of spike, and may contribute to attenuation by diminishing furin cleavage–dependent pathogenesis. The rVSV platform’s capacity for high titers, along with attenuation from G deletion and interferon sensitivity, supports a favorable safety and manufacturability profile. The observed Th1-biased isotype response addresses concerns of Th2-skewed vaccine-associated enhanced respiratory disease. Overall, the findings address the central goal of producing a safe, scalable, single-dose vaccine capable of protecting against SARS-CoV-2 disease in a relevant small animal model.
This work reports the generation and preclinical validation of rVSV-ΔG-spike, a replication-competent VSV-based SARS-CoV-2 vaccine. The vaccine exhibits authentic spike antigenicity, induces potent neutralizing antibodies after a single dose, confers protection against high-dose challenge in hamsters with rapid viral clearance and reduced lung pathology, and elicits a Th1-skewed response in mice. These attributes, together with high production titers, support advancement toward clinical evaluation. Future research should assess durability of protection, dose optimization and routes of administration, safety and efficacy in additional animal models and humans, and breadth of protection against variant spikes.
The study is preclinical, with efficacy demonstrated in golden Syrian hamsters and isotype profiling performed in mice due to reagent constraints; translation to humans remains to be shown. Follow-up duration was limited to 7–12 days post-challenge for pathology and weight, so durability of immunity and long-term safety were not assessed. The virus was adapted through passaging on Vero E6, acquiring spike mutations (R685G at S1/S2 and a 24-aa cytoplasmic tail truncation) that may affect antigen processing or pathogenesis relative to wild-type spike; while potentially beneficial for attenuation and production, their impact on breadth of immunity was not evaluated. Mucosal immunity and transmission-blocking efficacy were not directly measured.
Related Publications
Explore these studies to deepen your understanding of the subject.