Medicine and Health
A single-cell nanocoating of probiotics for enhanced amelioration of antibiotic-associated diarrhea
J. Pan, G. Gong, et al.
The human gut microbiota underpins gastrointestinal and systemic health, motivating the use of orally administered microbes (probiotics) to protect against pathogens, modulate immunity, influence nutrient absorption, and affect neurological outcomes. However, widespread antibiotic use is nonspecific, depleting commensals and causing dysbiosis associated with antibiotic-associated diarrhea (AAD), inflammation, allergies, and other conditions. Patients often take probiotics to restore microbial balance during antibiotic courses, but antibiotics also kill the probiotic strains, undermining efficacy. This challenge extends to fecal microbiota transplant (FMT) and other bacteriotherapies where coordinating antibiotic administration with microbial engraftment is difficult. Encapsulation approaches have been explored to improve survival and colonization, but a simple, safe, rapid, and broadly protective coating against diverse antibiotics remained unmet. The study proposes a biocompatible, plant-derived polyphenol-based nanoarmor (tannic acid coordinated with Fe(III)) that transiently coats individual probiotic cells to block antibiotic action while preserving bacterial viability and function.
Prior work has examined probiotic therapies, FMT for severe Clostridium difficile infections, and impacts of dysbiosis on health. Various encapsulation strategies (polymeric particles, biofilm-inspired coatings, layer-by-layer shells, hydrogel biocontainment) have improved survivability and delivery of probiotics through the GI tract. Metal–phenolic networks (e.g., TA–metal complexes) have been used as versatile, biocompatible coatings and functional biomaterials, binding diverse surfaces via multiple interactions. Despite these advances, broad-spectrum, rapidly applied, single-cell coatings that protect probiotics against multiple antibiotic classes during concurrent administration had not been established, motivating the current nanoarmor approach.
- Nanoarmor construction: Probiotic cells (Escherichia coli Nissle 1917, Lactobacillus casei ATCC393T, and a commercial 10-species blend, CVS HPC) were washed and suspended in PBS. FeCl3·6H2O and tannic acid (TA) solutions were sequentially added with brief vortexing to form a Fe(III)–TA supramolecular nanoshell on individual cells.
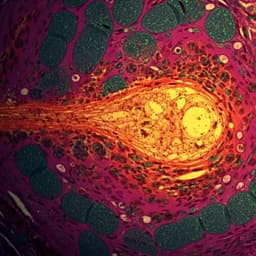
- Characterization: Coating formation and morphology were confirmed by confocal laser scanning microscopy (BSA–Alexa Fluor 647 labeling), TEM, SEM. Zeta potential measurements assessed surface charge shifts consistent with polyphenol coatings. XPS verified Fe–TA presence. BET nitrogen adsorption and cross-sectional TEM characterized microporosity (pore diameters ~2.34–10.86 nm).
- In vitro antibiotic protection: Armored and naïve bacteria were exposed for 24 h to six antibiotics (ciprofloxacin, tobramycin, neomycin, levofloxacin, norfloxacin, gentamicin) at excess minimum bactericidal concentrations (MBCs). Viability was quantified by CFU counts and post-exposure growth curves in LB/MRS.
- Mechanism studies: Quartz crystal microbalance (QCM) measured adsorption of antibiotics onto Fe(III)–TA-coated Au chips vs bare Au, inferring multiple molecular interactions (hydrogen bonding, hydrophobic, electrostatic). Antibiotic solutions were pre-incubated with Fe(III)–TA aggregates (no bacteria), then supernatants added to EcN cultures; CFUs and HPLC quantitated antibiotic depletion (>90% adsorption) to support an adsorption-based inactivation mechanism.
- Lyophilization and enteric delivery: Naïve and armored bacteria were lyophilized and packed into Eudragit L100 enteric capsules. Viability and growth post-lyophilization were measured. Simulated gastric fluid (pH 1.2, 2 h) and simulated intestinal fluid (pH 6.8, 12 h) models assessed release and survival with/without levofloxacin; recovery growth was monitored. Adhesion to rat intestinal mucus was tested; TEM assessed morphology after antibiotic exposure.
- In vivo rat study: Male Wistar rats received levofloxacin (2 g/L) in drinking water for 3 days, then daily oral gavage of enteric capsules containing 10 mg lyophilized E. coli consortium (EcCtet: EcN + BL21(DE3) with tetracycline resistance) as naïve or armored for 6 days, continuing levofloxacin during this period. After day 9, treatments ceased and monitoring continued to day 11. Control cohorts received bacteria without antibiotics. Daily fecal CFUs on tetracycline-selective plates quantified colonization. Body weight, stool appearance/score, fecal water content and Na+ (ICP-MS), and occult blood were assessed. At endpoint, GI segments (small intestine; colon proximal/medial/distal) were homogenized for CFUs; H&E histology assessed tissue morphology.
- Inflammation and gene expression: Serum cytokines (IL-6, IL-1β, TNF-α, IL-10) by ELISA; colonic gene expression by RT-qPCR (2^-ΔΔC method, GAPDH control) for pro- and anti-inflammatory cytokines and tight junction proteins (occludin, claudin-1).
- Metagenomics: For the probiotic mixture and healthy rat fecal microbiota, metagenomic sequencing (Illumina Novaseq 6000, Kraken2 taxonomic assignment) assessed phylogenetic diversity and relative abundance.
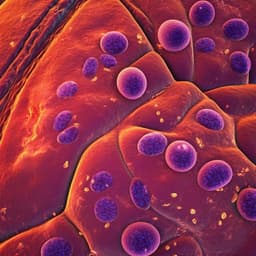
- Cytotoxicity: NIH3T3 cells treated with nanoarmor (100 µg/mL) for 24 h; apoptosis by Annexin V-FITC/flow cytometry.
- Statistics: Experiments repeated at least three times; data as mean ± SEM; ANOVA with multiple comparisons and two-tailed unpaired t-tests; significance thresholds as reported in figure legends.
- Coating formation: A uniform Fe(III)–tannic acid nanoarmor (~20 nm thick) formed around individual bacteria (EcN, L. casei, and a 10-species probiotic blend). Zeta potential shifted to more negative values; XPS confirmed Fe–TA presence. The nanoshell was microporous (pore diameters ~2.34–10.86 nm), excluding physical occlusion as the main protection mechanism.
- Broad-spectrum antibiotic protection in vitro: Armored EcN, L. casei, and the probiotic blend remained viable after 24 h exposure to six clinically relevant antibiotics at or above MBCs, whereas naïve counterparts showed no detectable CFUs. Post-exposure, armored cells resumed growth in fresh media; naïve cells did not. Metagenomics indicated that nanoarmor preserved CFUs and phylogenetic diversity of the probiotic consortium, with minor shifts in relative abundance.
- Mechanism—adsorptive inactivation: QCM showed substantial mass increases for all six antibiotics on Fe(III)–TA-coated substrates vs bare Au, indicating strong adsorption via multiple interactions. Pre-incubation of antibiotics with Fe(III)–TA aggregates protected EcN and HPLC quantified >90% depletion of antibiotics from solution, supporting an adsorption-based reduction of local antibiotic concentration around armored cells.
- Enteric delivery and GI simulation: Lyophilization did not impair viability or growth of naïve vs armored EcN. In simulated GI transit, enteric capsules protected contents in SGF and released them in SIF. In SIF with levofloxacin, armored EcN maintained significantly higher CFUs than naïve (p < 0.001); armored cells recovered and reached growth plateaus post-exposure, whereas naïve did not. Nanoarmor did not impair mucus adhesion.
- In vivo colonization under antibiotics: With levofloxacin, fecal CFUs of naïve EcCtet increased slowly to 2.84 × 10^6 CFU/g by day 9, whereas armored EcCtet rapidly increased from 2.60 × 10^6 to 12.56 × 10^6 CFU/g, peaking at 12.88 × 10^6 CFU/g on day 7 and remaining stable through day 11 (p = 0.001211). Without levofloxacin, both groups maintained lower CFUs (e.g., distal colon at endpoint: 0.96 × 10^6 CFU/g armored vs 0.73 × 10^6 naïve). With levofloxacin, endpoint distal colon CFUs were higher (6.40 × 10^6 armored vs 3.48 × 10^6 naïve CFU/g). Spatially, CFUs were low in small intestine and higher from proximal to distal colon.
- Mitigation of AAD symptoms: Levofloxacin induced weight loss; armored EcCtet reversed weight decline starting day 7 (p = 0.02189). Fecal consistency improved more rapidly with armored EcCtet (watery to normal; yellowish-brown to dark-brown). Fecal water content and Na+ levels decreased more with armored vs naïve treatment; no occult blood observed. ELISA showed lower serum pro-inflammatory cytokines (IL-6, IL-1β, TNF-α) and higher IL-10 with armored probiotics; RT-qPCR showed downregulation of pro-inflammatory colonic cytokine genes and upregulation of IL-10 and tight junction proteins (occludin, claudin-1).
- Safety: Histology showed normal GI tissue morphology across groups; no detrimental physiological effects. Armored EcCtet showed no significant toxicity at oral doses up to 20 mg/day. In healthy rats, armored probiotics did not significantly alter overall intestinal flora composition (minor relative abundance changes).
- Statistics: Multiple comparisons showed significant differences favoring armored groups across antibiotic protection assays and in vivo outcomes (numerous p-values < 0.01 or < 0.001 as reported).
The study addresses a central challenge in probiotic therapies: concurrent antibiotic administration undermines probiotic survival and function. A transient, biocompatible Fe(III)–tannic acid nanoarmor, applicable to both Gram-negative and Gram-positive bacteria and to multi-species consortia, broadly protected against antibiotics with diverse structures and mechanisms. Mechanistically, the nanoarmor adsorbs antibiotics through multiple noncovalent interactions, lowering local antibiotic concentration and preventing cellular uptake and killing. Protection persisted through simulated GI transit and during in vivo antibiotic exposure, enabling enhanced colonization, amelioration of antibiotic-associated diarrhea, and reduction of inflammatory markers, while maintaining safety. These findings suggest that nanoarmor can enhance the efficacy of probiotic regimens when timing with antibiotics cannot be precisely managed and could be extended to other therapeutic bacteria modalities (e.g., FMT, engineered consortia).
A metal–polyphenol (Fe(III)–tannic acid) single-cell nanoarmor provides a simple, safe, and rapid method to transiently protect probiotics from multiple antibiotics. It preserves viability and function in vitro, supports recovery after exposure, and enables enhanced colonization and therapeutic benefit in a rat AAD model, improving stool parameters and inflammatory profiles without detectable toxicity. The approach is broadly applicable across probiotic species and consortia. Future work could evaluate efficacy across additional antibiotic classes and dosages, optimize coating persistence and degradation kinetics in vivo, test diverse disease models (e.g., inflammatory bowel disease), and integrate with clinical bacteriotherapies such as FMT or engineered therapeutic microbes.
- The in vivo efficacy was demonstrated in a rat model with levofloxacin-induced dysbiosis; translation to humans and to other antibiotics/regimens requires further validation.
- Only six antibiotics were tested; broader antibiotic classes and pharmacokinetics in vivo were not exhaustively assessed.
- Outcomes were primarily short-term (up to 11 days); long-term colonization dynamics, microbiome recovery, and repeated dosing effects were not evaluated.
- Efficacy was shown for selected strains (EcN, L. casei, and a commercial blend); generalizability to other therapeutically relevant strains requires additional studies.
- While protection is transient and designed to dissipate with cell division, precise control over coating persistence in complex GI environments was not fully characterized.
Related Publications
Explore these studies to deepen your understanding of the subject.