Medicine and Health
A cyclic heptapeptide-based hydrogel boosts the healing of chronic skin wounds in diabetic mice and patients
Z. Fu, H. Sun, et al.
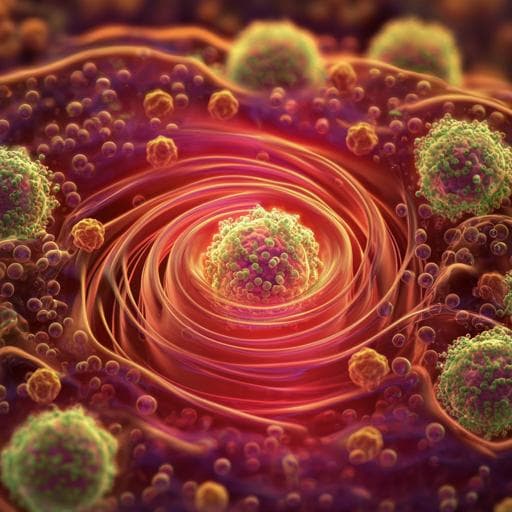
This groundbreaking research, conducted by Zhe Fu and colleagues, introduces CYRL-QN15, a revolutionary cyclic heptapeptide that significantly improves skin wound healing. Encased in a novel hydrogel, this treatment not only enhances cell growth and migration but also promotes vital immune responses, illustrating a powerful approach to tackling chronic skin wounds effectively.
Related Publications
Explore these studies to deepen your understanding of the subject.







