Biology
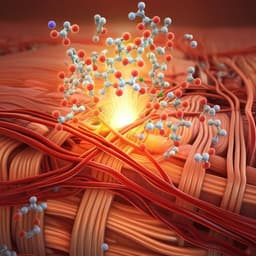
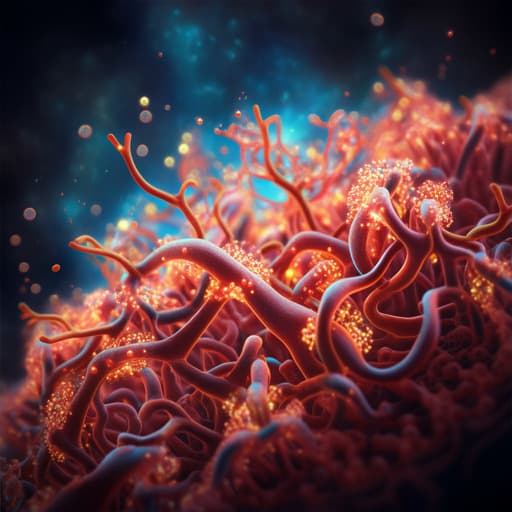
Transplanted human iPSC-derived vascular endothelial cells promote functional recovery by recruitment of regulatory T cells to ischemic white matter in the brain
B. Xu, H. Shimauchi-ohtaki, et al.
This groundbreaking research by Bin Xu, Hiroya Shimauchi-Ohtaki, Yuhei Yoshimoto, Tetsushi Sadakata, and Yasuki Ishizaki reveals how transplanting human iVECs can transform outcomes in ischemic stroke models, particularly by enhancing the recruitment of regulatory T cells and promoting myelin regeneration. Dive into the fascinating interplay between cellular therapies and neuroinflammation!
Related Publications
Explore these studies to deepen your understanding of the subject.