Medicine and Health
Tissue extracellular matrix hydrogels as alternatives to Matrigel for culturing gastrointestinal organoids
S. Kim, S. Min, et al.
The study addresses the dependency of gastrointestinal (GI) organoid culture on Matrigel and its limitations: tumor-derived origin, batch-to-batch variability, potential pathogen transmission, safety concerns, cost, and lack of GI tissue-specific microenvironment. The authors hypothesize that hydrogels derived from decellularized GI tissues (stomach and small intestine) can better recapitulate native ECM composition and mechanics, thereby replacing Matrigel for GI organoid culture by providing optimal cell–matrix cues for organoid development, function, long-term expansion, and transplantation utility.
The paper situates Matrigel as the standard but highlights its drawbacks: tumor origin, variability, safety/pathogen risks, and non-physiologic matrisome composition (glycoprotein-heavy, e.g., laminin-111). Prior alternatives include synthetic PEG hydrogels functionalized with RGD and protease-degradable peptides and natural matrices (alginate, fibrin) supplemented with ECM proteins; while supportive, these lack the biochemical complexity of native tissue ECM. Earlier decellularized intestine-derived matrices were explored but often used ionic detergents like SDC, potentially damaging ECM and reducing bioactivity. The authors propose optimized decellularization to preserve native matrisome complexity and test whether tissue-specific ECM hydrogels (SEM, IEM) can serve as effective, safer, and more reproducible substitutes.
- ECM source and decellularization: Porcine stomach and small intestine tissues were decellularized using two protocols. Optimized Protocol 1 (non-ionic Triton X-100 with NH4OH, low temperature, extended washes) preserved ECM components; Protocol 2 (ionic detergents such as SDC) achieved cell removal but reduced ECM (notably GAGs). Tissues were lyophilized post-decellularization.
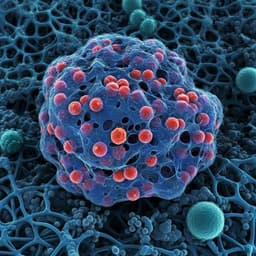
- Hydrogel preparation and characterization: Decellularized ECM was pepsin-digested in HCl, neutralized (PBS, NaOH), and thermally gelled at 37 °C. Ultrastructure was imaged by SEM; viscoelastic properties (storage modulus G′ at 1 Hz) measured by rheometry across concentrations. Endotoxin levels were quantified (chromogenic assay). In vitro immunogenicity was evaluated via TNF-α secretion from RAW 264.7 macrophages; in vivo biocompatibility assessed by subcutaneous injection in mice with H&E and toluidine blue staining.
- Proteomics: LC-MS/MS with MaxQuant/Andromeda pipeline; iBAQ for relative quantification; LFQ for piglet vs adult comparisons; PCA, Pearson correlations for batch/donor variability; mapping to Matrisome Project and Human Protein Atlas; GO/GOBP enrichment with g:Profiler/PANTHER.
- Organoid derivation and culture: Mouse gastric glands and small intestinal crypts isolated (EDTA chelation), embedded in SEM or IEM at varied concentrations to optimize conditions (gastric: 1–7 mg/ml; intestinal: 1–5 mg/ml). Standard Wnt/R-spondin/Noggin/EGF-based media used; passages every 4–7 days with collagenase IV for ECM hydrogel recovery (Matrigel via Cell Recovery Solution). Additional tests with colon organoids, hPSC-derived intestinal organoids, and GI tumoroids.
- Functional assays: Immunostaining for stemness (SOX9/Ki67) and differentiation markers (MUC5AC/CHGA/HK for gastric; MUC2/LYZ/CHGA/VILLIN for intestinal), tight junction (ZO1), ECAD; acridine orange acid secretion in gastric organoids; forskolin-induced swelling for CFTR function in intestinal organoids. YAP activation assessed by nuclear/cytoplasmic localization and RNA-seq target gene expression.
- RNA-seq: Organoids in SEM/IEM vs Matrigel, and native tissues; Novaseq platform; DEG criteria FC > 2, p < 0.05, FDR < 0.1; GO enrichment and comparison of ECM/cell–matrix interaction gene sets.
- Tissue specificity and age effects: ECM hydrogels from other tissues (skin, lymph, heart, muscle) compared for GI organoid support; piglet (2-month) vs adult pig (6-month) SEM/IEM compared for organoid outcomes and matrisome composition; supplementation of adult IEM with FN and/or TNC tested.
- Storage and cryopreservation: Pre-gel SEM/IEM stored at −80 °C (up to 6 months) or 4 °C (up to 1 month); post-thaw organoid formation and morphology assessed. Organoids cryopreserved within IEM vs Matrigel compared for viability and apoptosis (cleaved caspase-3).
- Transplantation: EGFP+ organoids in diluted TAMRA-labeled SEM/IEM (1:20) instilled into mouse models of acetic acid-induced gastric and intestinal injury; engraftment tracked at 0, 4, 7, 28 days; inflammatory response assessed (F4/80 macrophages).
- ECM preservation and mechanics: Optimized non-ionic decellularization removed cells while preserving ECM (GAG maintained) and yielded hydrogels with 1.6–3.3-fold higher storage modulus than ionic-detergent-prepared matrices. SEM and IEM showed nanofibrous ultrastructure akin to collagen I.
- Safety/biocompatibility: Endotoxin levels were low (SEM 0.344 ± 0.007 EU/ml; IEM 0.225 ± 0.016 EU/ml), below FDA 0.5 EU/ml limit; macrophage TNF-α release negligible; in vivo injections showed no necrosis/inflammation.
- Proteome differences vs Matrigel: Matrigel matrisome was >96% glycoproteins with only ~0.4% collagens and ~1% proteoglycans. SEM/IEM were collagen-rich (SEM: ~67% collagens, ~13% proteoglycans; IEM: ~51% collagens, ~26% proteoglycans), with 19–20 collagen subtypes detected; preserved GI tissue-enriched matrisome and non-matrisome proteins absent in Matrigel. Batch/donor variability was low: overlap of >100 matrisome proteins across donors (SEM 102; IEM 114), high PCA/pearson similarity.
- Optimal culture conditions: Gastric organoids formed across SEM 1–7 mg/ml; best efficiency at 5 mg/ml. Gene expression of stemness (Lgr5/Axin2) and differentiation (Pgc, Atp4a/b) in 5 mg/ml SEM comparable or higher vs Matrigel (e.g., Atp4b higher, p < 0.0001). Intestinal organoids formed in IEM 1–5 mg/ml; 2 mg/ml selected with higher Lgr5 (***p < 0.0001) and Muc2 (**p to ***p values) vs Matrigel.
- Phenotype/function: Gastric organoids in SEM and Matrigel had similar morphology and marker expression; size CV lower in SEM (66.7%) vs Matrigel (74.5%). Parietal cell presence/function evidenced by Atp4a/b, HK protein, ultrastructure (mitochondria/canaliculi), acridine orange acid accumulation similar across matrices, and histamine response. Intestinal organoids in IEM showed lower size CV (35.1% vs 47.7%), similar differentiation marker areas, and comparable CFTR function (forskolin-induced swelling).
- Transcriptomics: Compared to Matrigel organoids, SEM (gastric) had 590 DEGs (312 up, 278 down), IEM (intestinal) had 270 DEGs (213 up, 57 down). ECM and cell proliferation GO terms were upregulated; extracellular region/structure and cell–matrix adhesion gene sets more upregulated vs Matrigel. Several genes related to epithelial homeostasis and injury response (e.g., Procr, Mcpt2, Icam1, Cxcl10, Cxcl16, Timp3 in intestinal; Msi1, Dbn1, Chgb, Nrg1 in gastric) were expressed at levels closer to native tissues than Matrigel organoids. YAP signaling was more active in IEM (higher nuclear/cytoplasmic YAP; targets Ctgf, Ankrd1, Ereg, Cyr61 increased).
- Tissue specificity: SEM/IEM best supported GI organoids; non-GI ECMs (skin, lymph, heart, muscle) yielded lower viability, smaller, disorganized organoids, reduced formation efficiency and Lgr5 expression. Proteomics showed GI-critical matrisome proteins (e.g., COL6A3/A5/A6, FN1, laminins) higher in SEM/IEM vs skin ECM.
- Age effects: Piglet-derived SEM/IEM supported higher stemness marker expression (gastric: Lgr5, Axin2, Pgc, Atp4a/b significantly higher; intestinal: Lgr5, Olfm4 higher) with similar formation efficiency to adult ECM. Piglet ECM had higher levels of FBN2, FN1, TNC; adding FN to adult IEM increased Lgr5/Axin2, whereas TNC alone or FN+TNC did not further improve.
- Storage/cryopreservation: Pre-gel SEM/IEM retained organoid support after −80 °C storage up to 6 months or 4 °C up to 1 month with no differences in formation efficiency, morphology, or marker expression vs fresh. Organoids cryopreserved within IEM survived/thrived post-thaw better than in Matrigel; cleaved caspase-3+ area was 4.8-fold higher in Matrigel organoids (13.67%) than in IEM organoids (2.85%).
- Transplantation: EGFP+ gastric/intestinal organoids delivered with diluted (1:20) TAMRA-labeled SEM/IEM into acetic acid-injured mouse stomach/intestine engrafted efficiently and localized to injury sites at 4–28 days. ECM carriers alone showed negligible macrophage infiltration.
- Variability and cost: Proteomics indicates low batch/donor variability for GI ECMs under controlled sourcing; endotoxin and immunogenicity low; estimated cost lower than Matrigel (per supplementary).
The findings support that GI tissue-derived ECM hydrogels (SEM and IEM) better emulate native GI matrisome composition than Matrigel, enhancing cell–ECM signaling, ECM remodeling gene programs, and aspects of maturation and function in GI organoids. Collagen-rich matrices likely promote YAP activation and regenerative-like states in intestinal organoids, which could be advantageous for repair models. Tissue specificity matters: GI-derived ECMs outperform non-GI ECMs, highlighting the need to match organoid type to ECM origin. Age-related matrisome differences (e.g., higher FN1, FBN2, TNC in piglet ECM) correlate with higher stemness, suggesting tunable formulations or supplementation (FN) can improve adult ECM or inform chemically defined hydrogels. Practical benefits include long-term storage of pre-gel solutions, improved cryopreservation of organoids within ECM, and effective in vivo delivery/engraftment, addressing translational gaps left by Matrigel’s tumor origin and safety concerns. Overall, SEM/IEM enable organoids with gene expression closer to native tissue in ECM and injury-response pathways, supporting their use in disease modeling, drug testing, and regenerative applications.
GI tissue-derived ECM hydrogels (SEM, IEM) function as effective alternatives to Matrigel for gastric and intestinal organoid culture, supporting robust formation, appropriate differentiation and function, long-term passaging, and in vivo engraftment. Proteomics reveals GI-like matrisome complexity with low batch/donor variability and better alignment to native tissue than Matrigel. Age-related matrisome factors (e.g., fibronectin) enhance stemness and can be leveraged to optimize ECM formulations or design chemically defined hydrogels. The hydrogels store well and protect organoids during cryopreservation, improving practicality and scalability. Future work should: 1) define minimal, non-xenogeneic, chemically defined ECM compositions inspired by identified key matrisome components (e.g., collagens, decorin, biglycan, lumican, FN), 2) optimize conditions to enhance specific cell types (e.g., parietal and goblet cells to form mucus layers), 3) comprehensively validate with human GI organoids, and 4) conduct long-term functional transplantation studies to establish therapeutic efficacy.
- Source is xenogeneic (porcine), so while safer than tumor-derived Matrigel, full clinical translation requires additional safety/standardization and possibly human-derived or fully defined synthetic matrices.
- Intestinal organoids in IEM exhibited fewer buds, potentially reflecting a more fetal/regenerative or less mature architecture, despite comparable differentiation markers.
- Goblet cell numbers and surface mucus layer coverage were insufficient under standard conditions; additional media/culture strategies are required.
- Parietal cell proportion in gastric organoids remains lower than native tissue, indicating room for improved differentiation protocols.
- Transplantation studies were short to mid-term; long-term engraftment, integration, and functional recovery need further evaluation.
- Only selected ECM components (FN, TNC) were tested for supplementation and at limited concentrations; broader, systematic factor screening is needed.
- Human organoid data were limited; more extensive, long-term human studies are necessary.
Related Publications
Explore these studies to deepen your understanding of the subject.