Health and Fitness
Thoracic adipose tissue contributes to severe virus infection of the lung
F. Hornung, L. Schulz, et al.
This research conducted by Franziska Hornung and colleagues explores the surprising role of adipose tissue in the fight against respiratory viruses like influenza and COVID-19. The study reveals that while fat tissue can indirectly assist virus replication through inflammation, direct replication of SARS-CoV-2 in fat cells is absent. Discover how this could reshape our understanding of obesity's impact on viral infections.
~3 min • Beginner • English
Introduction
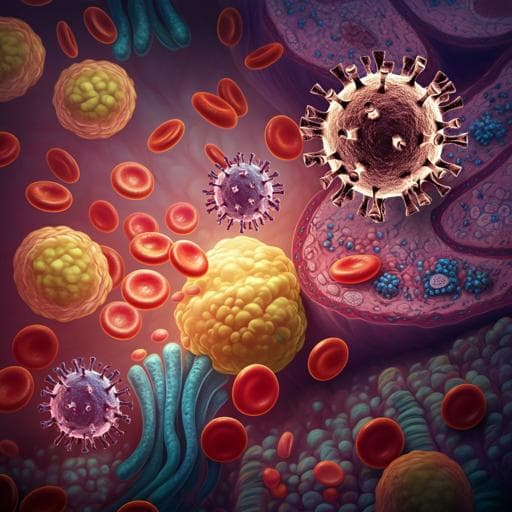
The emergence of novel respiratory viruses continues to cause outbreaks, exemplified by the 2009 influenza A (IAV) pandemic and the SARS-CoV-2 pandemic. Epidemiology has identified obesity as an independent risk factor for severe viral respiratory infections, in addition to age and immunosuppression, with higher BMI associated with increased COVID-19 mortality. Obesity, characterized by excess adipose mass, functions not only as an energy store but also as an endocrine organ with low-grade inflammation and macrophage-related proinflammatory gene expression. Mechanisms such as adipocyte death, chemotaxis, hypoxia, and fatty acid flux may drive macrophage infiltration in adipose tissue. The aim of this study was to investigate the role of adipose tissue in lung infections and test whether adipose tissue serves as a replication site for respiratory viruses, thereby contributing to disease severity in obesity.
Literature Review
Methodology
- Viral strains and titration: In vivo infections used IAV H1N1 Influenza A/Jena/5852/09 (pdmH1N1, HA-G222). In vitro IAV infections used A/Puerto Rico/8/34 (PR8) propagated in MDCK cells. SARS-CoV-2 variants: alpha (MW633324.1) and delta (ON650061.1) isolated at Jena University Hospital; omicron B.1.1.529 from EVA-G, propagated in Vero-ACE2 cells. Standard plaque assays performed on MDCK (IAV) or Vero-76 (SARS-CoV-2).
- Mouse models: Non-randomized, no blinding. DIO model: female BALB/cJRj mice (5 weeks) fed high-fat diet (60% fat kcal) for 12 weeks; obesity confirmed as mean(NFD weight)+3×SD criterion; excluded if unmet. ob/ob model: female C57BL/6 Lep ob/ob (homozygous) and ob/+ (heterozygous) controls. Intranasal infection under isoflurane with 10^? PFU HA-G222-mpJena/5258 (pdmH1N1). Body weight and burden scores measured daily for 21 days. Lung homogenates used for plaque assays and cytokines; thoracic and abdominal adipose tissues collected for RNA expression.
- Human tissues (COVID-19 autopsy): Early postmortem autopsies of SARS-CoV-2 omicron patients; multiple lung lobes and thoracic adipose depots (pericardial, epicardial, mediastinal) sampled. Ethics approvals provided.
- Human primary adipocytes: PromoCell human white preadipocytes differentiated per manufacturer. Mature adipocytes infected with IAV PR8 at MOI 1 (30 min adsorption; TPCK-trypsin added post-infection) and with SARS-CoV-2 alpha, delta, omicron at MOI 1 (60 min adsorption; cultured 1 and 3 days). Supernatants collected for plaque assays and cytokines; cells for IF and RNA/protein.
- Receptor analysis: Lectin staining with SNA (α2,6-linked sialic acid) and MAL II (α2,3-linked) on fixed adipocytes; visualization with streptavidin-Cy3 and phalloidin/Alexa Fluor 488.
- Co-culture: Mature adipocytes in bottom wells; human primary lung fibroblasts (IMR-90) seeded in transwells placed above adipocytes. Fibroblast side infected with IAV MOI 1; viral titers and cytokines measured at 24 h.
- Macrophages: PBMC-derived monocyte differentiation to macrophages; infected with IAV PR8 and SARS-CoV-2 delta/omicron. IAV infections with TPCK-trypsin; SARS-CoV-2 in RPMI+HSA. Time points at 8 h and 24 h p.i.; plaque assays, qRT-PCR (intra/extracellular RNA), cytokines, LDH cytotoxicity, and IF for dsRNA and CD68.
- Protein/RNA assays: Western blot for ACE2 and β-actin; qRT-PCR using SYBR Green for host genes (normalized to β-actin; ACE2 to Calu-3 positive control). Viral RNA via RIDA GENE kits for IAV M/NP/H1 and SARS-CoV-2.
- Cytokines: LEGENDplex human adipokine panel and COVID-19 cytokine storm panel; flow cytometric bead-based quantification.
- Histology/IF: H&E of mouse thoracic adipose; tissue IF staining for IAV NP and SARS-CoV-2 spike; phalloidin and DAPI counterstains. Cell IF with anti-dsRNA J2, and CD68 for macrophages.
- Statistics: GraphPad Prism 9; appropriate tests (Mann–Whitney, two-way ANOVA with Šidák/Tukey corrections, one-way ANOVA). Data as mean±SD or violin plots with medians; p-values reported in text and figure legends.
Key Findings
- Obesity increased severity and altered kinetics of influenza infection in mice:
- DIO mice: significant weight gain (p<0.0001), higher glucose (p=0.0015), increased abdominal adipose mass (p=0.0007), decreased lung weight; delayed peak weight loss (day 8) and incomplete recovery by day 21.
- ob/ob mice: higher body weight (p<0.0001), hyperglycemia (p<0.0001), increased adipose mass (p<0.0001), decreased lung weight (p=0.0042); delayed symptom onset and aggravated disease progression.
- Lung viral titers were significantly higher in DIO mice at day 4 p.i. (p<0.0001); ob/ob mice showed similar trend.
- Thoracic adipose tissue (TAT) is linked to influenza infection in vivo:
- ob/ob mice had more thoracic adipose tissue vs. controls at day 4 p.i. (p=0.0079).
- Elevated IAV RNA copies/mg detected in TAT of obese mice at day 4 p.i. (trend, p=0.0794).
- Proinflammatory cytokines upregulated in adipose tissue: IL-6 (ob/ob p=0.0108; DIO p=0.0444) and TNF-α (ob/ob p=0.0075; DIO p=0.0238); additional increases in thoracic adipose TNF-α (ob/ob p=0.0286) and IL-6 (DIO p=0.0079).
- IF staining detected IAV nucleoprotein in lung and thoracic adipose tissue at day 4 and day 21 p.i. in obese mice.
- Human primary adipocytes support IAV replication and mount antiviral responses:
- PR8 infection led to increased plaque titers at days 1 and 3 p.i. vs. mock.
- dsRNA detected in adipocytes at day 3 p.i., localized near lipid droplets; nuclear damage noted.
- Cytokine secretion increased: IFN-γ up at 24 h (p=0.0329); MCP-1 (p=0.0006) and IP-10 (p=0.0079) up at 72 h.
- Co-culture with lung fibroblasts did not change viral titers but increased IL-8 at 24 h p.i. (p=0.0153), suggesting enhanced inflammatory milieu.
- Adipocytes expressed predominantly α2,6-linked sialic acids, consistent with susceptibility to human IAV.
- SARS-CoV-2 presence in thoracic adipose tissue in humans but no replication in adipocytes in vitro:
- In five COVID-19 decedents (omicron), SARS-CoV-2 RNA detected across lung lobes and in thoracic adipose depots; highest loads in left lower lobe and mediastinal adipose.
- IF showed spike protein in mediastinal adipose; potential colocalization with macrophage marker CD68.
- Mediastinal adipose had higher IL-6 (p=0.0026), G-CSF (p=0.0001), and MCP-1 (p=0.0001) than lung tissue; IP-10 increased (ns).
- In vitro, adipocytes exposed to SARS-CoV-2 alpha and delta showed detectable titers at day 1 but declined by day 3 (alpha and delta, p<0.0001 for decline in delta); no dsRNA detected for alpha/delta/omicron.
- ACE2 mRNA and protein were not detectable in adipocytes relative to Calu-3 controls.
- Macrophages and inflammation:
- Monocyte-derived macrophages showed detectable IAV and SARS-CoV-2 (delta) at 8 h p.i.; only IAV remained at 24 h; intra/extracellular viral RNAs did not increase over time.
- dsRNA for IAV and SARS-CoV-2 observed in macrophages by IF.
- Omicron-infected macrophages had elevated MCP-1 (p=0.0012), IL-8 (p=0.0007), IP-10 (p=0.0003) at 24 h, and increased cytotoxicity with IAV (p=0.0424) and omicron (p=0.0063).
Discussion
The study addressed whether adipose tissue contributes directly to the pathogenesis of respiratory viral infections and helps explain the obesity-associated risk. Using two murine models, obesity was associated with delayed and more severe influenza disease courses and higher lung viral titers, indicating impaired viral control. Critically, influenza virus was detected in thoracic adipose tissue adjacent to lungs, and human primary adipocytes supported productive IAV replication with antiviral and proinflammatory responses. These findings support the concept that thoracic adipose tissue provides a proximate niche that can harbor and amplify respiratory viruses, potentially prolonging infection and contributing to elevated viral loads and extended shedding in obese hosts.
In contrast, while SARS-CoV-2 RNA and spike protein were present in thoracic adipose tissue of COVID-19 decedents and the local adipose milieu was highly inflamed, human adipocytes lacked ACE2 and did not support active replication of alpha, delta, or omicron variants. Macrophages within adipose tissue showed evidence of viral RNA and mounted robust inflammatory responses, implicating them as key mediators of adipose-associated inflammation during COVID-19. Thus, for IAV, both adipocytes and macrophages can contribute directly, whereas for SARS-CoV-2, adipose macrophages likely account for viral presence and inflammatory amplification rather than adipocytes themselves.
These results suggest that thoracic adipose tissue may be an underappreciated reservoir that shapes disease severity and duration for certain respiratory viruses, particularly in obesity. Targeting adipose tissue viral niches and the associated inflammatory responses could represent new therapeutic avenues to mitigate severe outcomes.
Conclusion
This work identifies thoracic adipose tissue as a contributor to respiratory viral infection severity. In obesity, thoracic adipose tissue adjacent to the lung can harbor influenza virus, with human adipocytes supporting IAV replication and secreting proinflammatory mediators, while adipose macrophages further amplify inflammation. For SARS-CoV-2, viral RNA and spike are present in thoracic adipose tissue in patients, but human adipocytes do not support replication in vitro, pointing instead to macrophages as key inflammatory players. These findings highlight adipose tissue as a potential viral niche influencing disease course in obesity.
Future research should develop and test interventions to reduce or eliminate viral reservoirs within thoracic adipose tissue, modulate adipose tissue inflammation, and delineate mechanistic pathways governing virus–adipose interactions across variants and host metabolic states.
Limitations
- Use of different influenza virus strains between in vivo (mouse-adapted pdmH1N1) and in vitro (PR8) experiments may limit direct comparability across systems.
- Animal studies were non-randomized and unblinded, introducing potential bias.
- Autopsy analysis included a small sample size (n=5 COVID-19 patients), limiting generalizability.
- Plaque assays for omicron were not feasible due to weak cytopathic effects, constraining direct quantification of infectious particles.
- In vitro primary cell models may not fully recapitulate complex in vivo adipose tissue microenvironments and cellular compositions.
Related Publications
Explore these studies to deepen your understanding of the subject.