Medicine and Health
The establishment of COPD organoids to study host-pathogen interaction reveals enhanced viral fitness of SARS-CoV-2 in bronchi
L. L. Y. Chan, D. E. Anderson, et al.
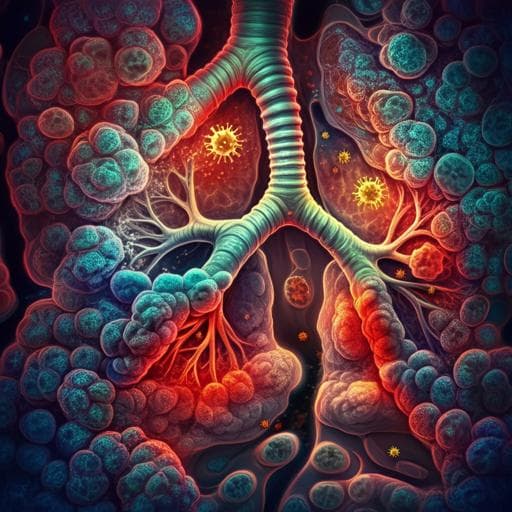
The study addresses the need for individualized in vitro models to investigate host-pathogen interactions in chronic obstructive pulmonary disease (COPD), a heterogeneous and complex respiratory disorder characterized by progressive airflow limitation, structural abnormalities, and frequent exacerbations. Traditional animal models fail to capture human genetics/epigenetics and the diverse endophenotypes seen in COPD. The authors propose developing patient-derived airway organoids (nasopharyngeal and bronchial) that reproduce the airway microenvironment at the individual level. These models aim to enable precision investigations of infection responses, particularly to viruses (e.g., SARS-CoV-2) and bacteria (e.g., Pseudomonas aeruginosa and Streptococcus pneumoniae), and to explore mechanisms underlying the observed worse COVID-19 outcomes in COPD.
Recent advances have enabled generation of stem cell-derived organoids that incorporate multiple cell types in three-dimensional architecture, recapitulating tissue-specific functions. Human airway organoids have been derived from nasal, bronchial, and alveolar tissues using adult or pluripotent stem cells and used to study diseases such as lung cancer and cystic fibrosis, and infections including RSV, enteroviruses, Cryptosporidium, influenza, and SARS-CoV-2. Epidemiology suggests COPD is associated with more severe COVID-19 outcomes, but mechanistic understanding is limited. Bacterial infections, notably by Streptococcus pneumoniae and Pseudomonas aeruginosa, are key contributors to COPD exacerbations. This background supports the development and application of COPD organoids to study host-pathogen interactions and disease-specific responses.
- Subject recruitment: 28 individuals (10 non-COPD healthy; 18 COPD) provided samples for organoid cultivation. COPD defined by GOLD criteria; exacerbation frequency categorized (non-exacerbator, exacerbator, frequent exacerbator). Ethics approvals obtained across institutions.
- Sample collection: Nasopharyngeal epithelial cells (HNPECs) obtained via flocked swabs; human bronchial epithelial cells (HBECs) obtained from surgical resections/bronchoscopy brushings.
- Cell culture and differentiation: HNPECs/HBECs expanded; seeded on transwells; differentiated at air-liquid interface (ALI) for 18 days; detached and embedded in Matrigel; expanded in Airway Organoid (AO) medium with R-spondin-1, FGF7, FGF10; then further differentiated at ALI for 4–6 weeks to form nasopharyngeal (NPOs) and bronchial organoids (BOs). Apical-out organoids generated via EDTA Matrigel solubilization and suspension culture in ultra-low attachment plates.
- Characterization: Immunofluorescence for TP63 (basal), SCGB1A1 (club), acetylated-α-tubulin (ciliated), MUC5AC (goblet), and ACE2. qRT-PCR for TP63, SCGB1A1, FOXJ1, MUC5AC and SARS-CoV-2 entry factors (ACE2, TMPRSS2, Furin, Neuropilin-1). Micro-optical coherence tomography (µOCT) used to visualize motile cilia and quantify ciliary beat frequency (CBF).
- SARS-CoV-2 infection: Three strains used: clade L ancestral Wuhan strain hCoV-19/Singapore/2/2020 (L-WU; EPI_ISL_407987), clade O hCoV-19/Singapore/1003/2020 (O-614D; EPI_ISL_574486), clade G D614G variant hCoV-19/Singapore/1005/2020 (G-614G; EPI_ISL_574489). Apical-out organoids infected at MOI 0.1 for 1 h, washed, re-embedded in Matrigel. Supernatants collected at 1, 24, 48, 72, 96 hpi for titration; lysates at 48 and 72 hpi for qPCR of viral N gene and host cytokines.
- Viral quantification: TCID50 on Vero-E6 cells using Karber method. qRT-PCR for viral N gene and host cytokines (IL-6, IFN-β, CXCL10, TNF-α). Cytokine proteins in supernatants measured by multiplex Luminex.
- Bacterial infection: Pseudomonas aeruginosa PAO1 and Streptococcus pneumoniae INS-E611 (serotype 6B) prepared; apical-out NPOs infected in suspension (1 h), washed, re-embedded; supernatants at 6 hpi for cytokines; lysates for qPCR of bacterial genes (P. aeruginosa 16S, S. pneumoniae lytA) and host cytokines/chemokines (CCL2, CCL5, CXCL10, TNF-α, IL-1β, IL-6, IL-8). Protein quantification by Luminex.
- Single-cell RNA-seq: Organoids dissociated; 10x Genomics Chromium (3' v3.1) libraries sequenced (HiSeq2500). Cell Ranger 6.0.2 alignment to GRCh38; Seurat 4.0 for QC, integration, clustering (resolution 0.3), UMAP visualization; DEGs via Wilcoxon tests; pathway analysis via IPA and GSEA. Pseudotime with Monocle3, using cycling basal cells as root.
- Bulk RNA-seq (bacterial study): ND and COPD NPOs mock or PAO1-infected (6 h); libraries via TruSeq Stranded mRNA; sequenced PE100; trimmed with Trimmomatic; aligned with Rsubread to GRCh38; counts with featureCounts; DESeq2 for DEGs (|log2FC|>1, adj p<0.05); clustering and GO with VISEAGO.
- Statistics: Normality testing (K-S test); t-test/ANOVA for normal data; Wilcoxon/Mann-Whitney/Kruskal-Wallis for non-normal; Spearman correlations. Significance at p<0.05.
- Organoid establishment and baseline characterization: • Both NPOs and BOs formed well-differentiated spheroids with basal, club, goblet, and ciliated cells. BOs were more ciliated, with higher FOXJ1 expression, and higher TP63 and SCGB1A1 by qPCR than NPOs.
- COPD organoid phenotype: • COPD NPOs/BOs showed goblet cell hyperplasia with significantly elevated MUC5AC expression versus non-diseased (NPO-ND vs NPO-COPD p=0.0004). • MUC5AC expression increased with exacerbation frequency (ND vs NE p=0.0117; ND vs E <0.0001; ND vs FE <0.0001). • MUC5AC inversely correlated with lung function (FEV1% predicted): Spearman R = -0.5890; p = 0.0008. • COPD BOs had significantly reduced ciliary beat frequency compared to non-diseased (p=0.0008).
- Single-cell RNA-seq: • Organoids recapitulated major airway epithelial cell populations. COPD organoids had fewer cycling basal (5.4% vs 16.0%) and ciliated epithelial cells (3.2% vs 5.2%), but more basal (45.7% vs 35.6%) and goblet cells (15.9% vs 11.5%). Club cells were similar (~29%). • COPD-specific over-representation of subpopulations: Basal cells 2 (35.3% vs 4.7%), Club cells 2 (15.6% vs 1.2%), Goblet cells 2 (10.4% vs 0.7%). Altered developmental trajectory from cycling basal cells toward ciliated/goblet lineages in COPD. • Enriched COPD pathways included mitochondrial dysfunction, ER stress, cilium reorganization, ECM remodeling, and proinflammatory signaling; patterns were consistent with public COPD datasets (e.g., GSE162154). Sirtuin signaling and oxidative phosphorylation changes noted.
- SARS-CoV-2 infection in non-diseased organoids: • L-WU and G-614G replicated in NPOs and BOs; O-614D failed to replicate in organoids (but did in Vero-E6). • In NPOs, G-614G reached higher titers than L-WU at 96 hpi and up to 168 hpi. • G-614G elicited stronger proinflammatory responses at 72 hpi: increased IFN-β, CXCL10, TNF-α in NPOs; increased IL-6 and IFN-β in BOs; CXCL10 protein increased in both.
- SARS-CoV-2 infection in COPD organoids: • Infectivity at 48–72 hpi comparable between COPD and non-diseased. • Enhanced replication in COPD BOs for both L-WU and G-614G (e.g., BO L-WU 24 hpi p=0.0110; 96 hpi p=0.0152; BO G-614G 24 hpi p=0.0294; 96 hpi p=0.0457). L-WU replicated less efficiently in COPD NPOs. • Following G-614G infection, COPD BOs exhibited reduced IL-6 and IFN-β expression compared to non-diseased BOs at 72 hpi (IL-6 p=0.0237; IFN-β p=0.0248), with a trend toward reduced CXCL10, suggesting impaired antiviral responses.
- Bacterial infection (NPOs): • ND and COPD NPOs had similar susceptibility to P. aeruginosa and S. pneumoniae by bacterial gene qPCR. • COPD NPOs showed greater proinflammatory responses at RNA and protein levels after P. aeruginosa infection (e.g., increased CCL2, CXCL10, IL-6 by qPCR; elevated CCL2, CCL4, CXCL10, TNF-β, IFN-γ, IL-6, IL-8, IL-9, GRO-α, G-CSF by Luminex; multiple comparisons p<0.05 to p<0.0001). • Bulk transcriptomics revealed in COPD NPOs (baseline) reduced ciliary movement and increased secretory/ECM remodeling; upon infection, COPD NPOs exhibited heightened inflammatory and stress responses compared to ND.
The established COPD airway organoids capture hallmark disease phenotypes—goblet cell hyperplasia, reduced ciliary beat frequency, and altered epithelial differentiation—validating them as physiologically relevant models that reflect individual donor pathology. The enhanced replication of SARS-CoV-2, particularly the D614G variant, in COPD bronchial organoids, alongside reduced interferon (IFN-β) and IL-6 responses, provides mechanistic insight into the observed clinical vulnerability of COPD patients to severe COVID-19, especially involving the bronchi. Single-cell analyses reveal intrinsic epithelial defects in COPD, including mitochondrial dysfunction and disrupted differentiation trajectories, which likely contribute to impaired antiviral immunity and exaggerated inflammatory responses. The organoids also model COPD responses to bacterial pathogens, showing amplified inflammatory signaling despite comparable bacterial loads, consistent with clinical exacerbation patterns. Overall, these findings address the research question by demonstrating that patient-derived COPD organoids are suitable platforms for dissecting host-pathogen interactions at the individual level, linking epithelial-intrinsic defects to infection outcomes, and supporting precision medicine approaches.
This work establishes and characterizes patient-derived nasopharyngeal and bronchial COPD organoids that recapitulate disease-specific epithelial structure and function. The models reveal enhanced SARS-CoV-2 replication competence and blunted interferon responses in COPD bronchi, offering cellular correlates for severe COVID-19 in COPD. They also demonstrate heightened inflammatory responses to common bacterial pathogens. These organoids enable individualized assessment of infection biology and therapeutic responses, with potential applications in high-throughput screening and pandemic preparedness. Future work should expand sample sizes, include paired upper and lower airway sampling per donor, integrate immune and vascular components, and apply single-cell analyses to infected organoids to further elucidate cell-type-specific host-pathogen dynamics.
- Nasopharyngeal and bronchial samples were obtained from different donors rather than paired from the same individuals.
- Healthy donors were relatively younger than COPD donors, introducing potential confounding.
- scRNA-seq analyses were based on one line per group (pooled NPO/BO), limiting generalizability; validation with larger cohorts is needed.
- Organoids lack immune and vascular components, reducing model complexity relative to in vivo tissue.
- scRNA-seq of SARS-CoV-2–infected organoids was not performed due to safety and logistics constraints.
Related Publications
Explore these studies to deepen your understanding of the subject.