Medicine and Health
System characterization of a human-sized 3D real-time magnetic particle imaging scanner for cerebral applications
F. Thieben, F. Foerger, et al.
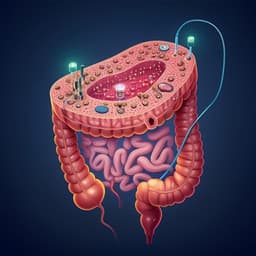
The study addresses the need for bedside, radiation-free, high-temporal-resolution neuroimaging suitable for intensive care units (ICUs). Conventional CT entails ionizing radiation and is impractical for frequent monitoring, while MRI has limited accessibility, long scan times, and encapsulates patients, complicating monitoring. Portable low-field MRI has shown promise, but Magnetic Particle Imaging (MPI) offers background-free, quantitative imaging with high temporal resolution, compact size, and compatibility with ICU environments. The clinical targets include neurovascular conditions such as ischemic stroke, intracranial hemorrhage, and traumatic brain injury that demand rapid diagnosis and monitoring. The research question is whether a human-sized MPI brain scanner can safely deliver 3D real-time imaging with sufficient sensitivity and spatial/temporal resolution for cerebral applications, including perfusion assessment, under realistic constraints like low power consumption and unshielded environments.
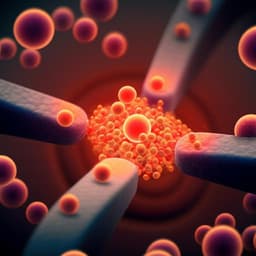
The paper situates the work within ongoing efforts to scale MPI from preclinical systems (small rodents) to human-sized scanners for head and extremities. MPI provides background-free contrast by exploiting the nonlinear magnetization response of magnetic nanoparticles and has demonstrated high spatiotemporal resolution, with reports up to 46 volumes per second. Prior applications in animal models include hyperthermia treatment, stem cell labeling, detection of lymph node metastasis, gut bleeding, lung perfusion, and cancer detection, as well as interventional guidance such as catheter steering and stent positioning. Multi-contrast (multi-color) MPI can encode particle properties (e.g., binding state, core size, orientation), environmental parameters (viscosity, temperature), and supports tracer discrimination. Earlier human head MPI prototypes established feasibility for 2D imaging; however, clinical translation requires improved 3D capability, sensitivity, resolution, safety (SAR, PNS), and manageable power consumption without heavy electromagnetic shielding. This work builds on and updates an earlier human-sized head scanner with redesigned hardware to enable 3D imaging and enhanced safety.
System overview: The scanner comprises (1) operational control (synchronized DAC/ADC via three RedPitaya STEMlab 125-14 boards, open-source software stack with GUI, surveillance unit for safety), (2) field generation (two orthogonal drive-field coils in x and z, and a dynamic selection-field generator moving the field-free point along y), (3) signal reception (dedicated receive coils in x and y with band-stop filtering and custom low-noise amplification), and (4) data processing (system matrix-based reconstruction and perfusion parameter computation). Field generation: Two orthogonal drive-field coils (DFCs) in x (solenoid) and z (saddle) are nested and constructed using Rutherford-parallelized Litz wire to reduce inductance and resistance, enabling high currents at low voltages. Drive fields are 5 mT (x) and 4 mT (z) at ~25.699 and 26.042 kHz, forming a 2D Lissajous trajectory in the xz-plane. A high-current resonator (HCR) with temperature-controlled capacitors tunes resonance; an inductive coupling network (toroidal air-core transformer) provides current gain, floating potentials, and symmetry. Residual coupling between DFCs (k≈0.06) is mitigated using a series decoupling capacitor network achieving −35 dB residual coupling. Transmit chains include a 5th-order differential band-pass filter to suppress harmonics (−65/−100/−150 dB for 2nd/3rd/4th harmonics) and an iron-core impedance-matching transformer. Two 1200 W power amplifiers drive the DFs, with feedback coils monitoring amplitude/phase (<1% control error). The selection-field generator (two coils on a soft-iron yoke, 200 mH each) produces a gradient with FFP motion along y (±43 mm) using AF Techron current-mode amplifiers (~380 W total). Identical 10 A DC yields gradients of 0.24 T/m in y and −0.12 T/m in x and z. Signal reception: Two dedicated receive coils are used: a gradiometric x-coil (10 turns plus 18 counter turns) and a y-direction saddle coil (2×20 turns). A 4th-order differential notch filter (20–33 kHz stopband) suppresses DF feedthrough; early stages use air-core coils to avoid nonlinearity, later stages use ferrite cores. A matching transformer precedes a custom low-noise amplifier (parallel JFET front-end followed by op-amp stages), then differential signaling to ADCs; an instrumentation amplifier generates single-ended measurement signals. Receive-path transfer functions are calibrated; resonances around 531 kHz (x) and 414 kHz (y) enhance higher harmonics. A send-receive (TxRx) pickup within the HCR exists but was inferior to dedicated receive coils for this system and not used for reconstruction. Imaging sequence: 3D imaging is achieved by superimposing the xz Lissajous DF trajectory with a slow triangular sweep of the selection field along y (4 Hz), sampling a nominal 3D FOV of approximately 84×85×67 mm³ with uniform slice spacing in y (~1.982 mm) and adequate in-plane sampling (largest Lissajous gap ~1.819 mm). The triangular sweep ensures periodicity, constant velocity, and reduced mechanical stress and PNS risk. Field analysis: Magnetic field profiles of DF and SF were measured on spherical designs using a 3D coil sensor (for DF) and a 3-axis Hall probe (for SF) to derive spherical harmonic expansions, assess homogeneity, quantify THD (0.0669% x, 0.127% z), and relate currents to gradient strength and FFP position. The measured DF FOV was approximately 83×80×73 mm³. System matrix acquisition and analysis: A robot-positioned 200 μL sample (Resotran, 8.5 mg/mL) was measured over a 15×15×11 grid covering 140×110×100 mm³; at each position a full 3D sequence (0.248 s) was acquired. Background measurements were acquired by moving the sample outside the bore. DF feedback stability showed <0.4% SD across 2491 measurements. System matrix rows were analyzed in frequency space under two interpretations: multi-patch (85 y-positions) and single-patch (continuous 3D), showing wave-like patterns, spatial shifts with patch movement, and the effect of field imperfections. Sensitivity experiment: A dilution series of Resotran in 50 μL volumes within 200 μL tubes (4–512 μg iron) was measured at three y-positions using a single 3D sequence per sample. Reconstructions used background subtraction; quantitative iron content was estimated by summing reconstructed concentration in a masked region and scaling to the system-matrix calibration. Spatial resolution experiment: Two 200 μL 8.5 mg/mL samples were imaged; one fixed at FOV center, the other robot-positioned with increasing edge-to-edge separation in 0.5 mm steps along x, y, z. Single-frame reconstructions on an interpolated grid (25×25×19) were assessed via line profiles; resolution was defined by a dip below half-maximum at the midpoint (and also reported for quarter-maximum). Dynamic perfusion experiment: A dual-hemisphere flow phantom was constructed from two 50 mL cylinders filled with 1 mm glass spheres, each with perforated inlet/outlet rods to mimic tissue perfusion. Two independent peristaltic pumps controlled flows. Five runs simulated 0%, 25%, 50%, 75%, and 100% stenosis in the left hemisphere by reducing its flow, while the right hemisphere was kept at 100 mL/min. A 100 μL bolus of pure Resotran (28 mg/mL) was injected. Each run collected 150 frames (37.2 s) using the 3D sequence. DF feedback stability showed <0.3% SD across frames. Reconstructions (single-patch approach) used an interpolated grid of 25×25×18 voxels. Perfusion image calculation: Post-processing included (i) selection of frames covering first-pass bolus, (ii) voxel-wise Hann low-pass filtering (10-sample window) and DC offset removal, (iii) threshold masking to exclude voxels below 10% of peak, (iv) voxel-wise computation of time-to-peak (TTP), mean-transit-time (MTT as FWHM), relative cerebral blood flow (rCBF as peak positive temporal gradient), and relative cerebral blood volume (rCBV as AUC over positive concentration). Relative measures were used due to lack of an arterial input function. Multi-contrast experiment: Two 200 μL samples of Resotran and synomag (8.5 mg/mL each) were positioned 50 mm apart. Two system matrices (one per tracer) were measured on a 15×15×1 grid in the xy-plane (FOV 140×110 mm²). A single 3D-sequence frame was acquired and reconstructed with two-channel Kaczmarz inversion to separate tracer signals, with background subtraction. Operational control and safety: An Arduino-based surveillance unit monitors temperatures and states, controls relays, and can interrupt transmission. Hardware interlocks and software control prevent unintended high DF levels; the resonant transmit chain is frequency-specific and self-limiting upon detuning. Floating potentials via transformers reduce shock risk; dielectric isolation is provided by the DFG housing. Total power consumption is below 4 kW. PNS considerations limited DF amplitudes to 5 mT (x) and 4 mT (z); selection-field slew rates (~24 T/m/s) are well below PNS thresholds. All experiments used phantoms.
- Achieved 3D single- and multi-contrast MPI at 4 Hz frame rate over a nominal head-sized FOV (~84×85×67 mm³), sampling a volume of ~480 mL.
- Field characterization: With 10 A SF coil currents, measured gradients were ~0.24 T/m in y and −0.12 T/m in x and z; DF THD was 0.0669% (x) and 0.127% (z). The measured DF FOV was ~83×80×73 mm³.
- System matrix: Frequency-space analysis showed expected wave-like patterns with spatial shifts across y-patches; single-patch interpretation improved SNR via longer Fourier windows and captured 3D encoding including y-oscillations. Field imperfections produced slight pattern distortions and rotations.
- Sensitivity: Detection limit was 8 μg iron (50 μL Resotran). At 4 μg, reconstructions showed position-independent background artifacts, indicating the limit. Quantitative reconstructions matched applied iron mass at higher levels, with underestimation below ~32 μg.
- Spatial resolution (half-maximum criterion): y-direction 6.7 mm, x-direction 11.2 mm, z-direction 31.2 mm. Quarter-maximum criteria yielded larger separations; results are consistent with gradient strengths and receive coil configurations.
- Dynamic perfusion: First-pass bolus imaging at 4 Hz successfully differentiated five stenosis levels (0–100% in 25% steps). Perfusion maps showed increasing TTP and MTT with stenosis and decreasing rCBF and rCBV in affected hemisphere; threshold masks highlighted reduced perfused area with increasing stenosis.
- Multi-contrast: Successful tracer discrimination and localization of Resotran and synomag in a two-dot phantom; minor channel leakage from Resotran into the synomag channel was observed but small relative to synomag’s intrinsic signal.
- Safety and operation: Imaging performed within peripheral nerve stimulation thresholds; total power consumption <4 kW; open-source control and reconstruction stack enabled live monitoring, with demonstrated online reconstruction latency <1 s (retrospective reconstructions reported).
The results demonstrate that a human-sized MPI brain scanner can provide real-time 3D imaging at 4 Hz with sufficient sensitivity (8 μg iron) and spatial resolution (best along y at ~7 mm) to capture hemispheric perfusion dynamics and differentiate graded stenoses in a head-sized phantom. The findings address the core objective of enabling bedside neuroimaging compatible with ICU constraints: the system operates with modest power, in unshielded environments, and within human PNS limits. The measured gradients and field profiles, together with system matrix analyses, explain the anisotropic resolution—best along y due to stronger gradients and a dedicated receive channel, moderate along x due to lower gradient but dedicated reception, and lowest along z without a dedicated receive coil. The dynamic perfusion study underscores the scanner’s capability to quantify temporal hemodynamic parameters (TTP, MTT, rCBF, rCBV) over a 3D volume at clinically relevant flow rates. Multi-contrast imaging further expands potential applications by discriminating tracers, enabling functional readouts (e.g., temperature, viscosity) or multi-parametric studies. Operational safety features, floating potentials, and low voltages near the patient support a pathway to human studies. While brain angiography-level resolution is not yet achieved, the present performance is a substantial step toward clinical utility for monitoring neurovascular conditions at the bedside.
This work presents and comprehensively characterizes a human-sized 3D real-time MPI brain scanner. The system achieves 4 Hz volumetric imaging with demonstrated sensitivity (8 μg iron), anisotropic but practical spatial resolution (approximately 7–12 mm in-plane and ~31 mm through-plane), and perfusion imaging capabilities that distinguish graded stenoses in a cerebral phantom. Multi-contrast imaging with clinically approved and MPI-tailored tracers was demonstrated. The scanner integrates open-source control and reconstruction software, robust safety mechanisms, and low power consumption suitable for unshielded ICU environments. Future directions include: adding a dedicated z-receive coil to improve through-plane resolution; optimizing field homogeneity and selection-field generators (e.g., multi-coil iron-core arrays) to enlarge the FOV and enable more flexible sequences; exploiting sequence redundancy to double frame rates; reducing online reconstruction latency; conducting animal and human studies to validate safety and performance; and leveraging clinically approved, MPI-tailored tracers to further improve sensitivity and resolution for applications like stroke assessment and hemorrhage detection.
- All experiments were performed on phantoms; safety, tolerability, and performance in humans remain to be validated in animal/human studies.
- Spatial resolution, particularly along z (~31 mm without a dedicated receive coil), is insufficient for detailed cerebral angiography.
- Sensitivity appears lower than an earlier 2D head scanner largely due to 3D sampling, shorter sequence length, and tracer differences; direct comparison is not feasible.
- Field imperfections (coil coupling, inhomogeneities, eddy currents) distort trajectories and system matrix patterns, potentially degrading image quality.
- Minor channel leakage observed in multi-contrast reconstruction requires further investigation.
- Quantitative measures at low iron masses (<32 μg) are underestimated; reconstructions may exhibit structured artifacts due to regularization and noise.
- Reported system-characterizing values lack formal accuracy estimates, though experiments were repeated to ensure qualitative reproducibility.
Related Publications
Explore these studies to deepen your understanding of the subject.