Medicine and Health
Synergy of pandemics-social isolation is associated with worsened Parkinson severity and quality of life
I. Subramanian, J. Farahnik, et al.
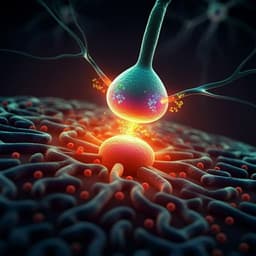
This research by Indu Subramanian, Joshua Farahnik, and Laurie K Mischley reveals a compelling link between social isolation and the severity of Parkinson's disease symptoms, impacting the quality of life for patients. Discover how maintaining social connections can be crucial, especially during social distancing measures.
Related Publications
Explore these studies to deepen your understanding of the subject.