Biology
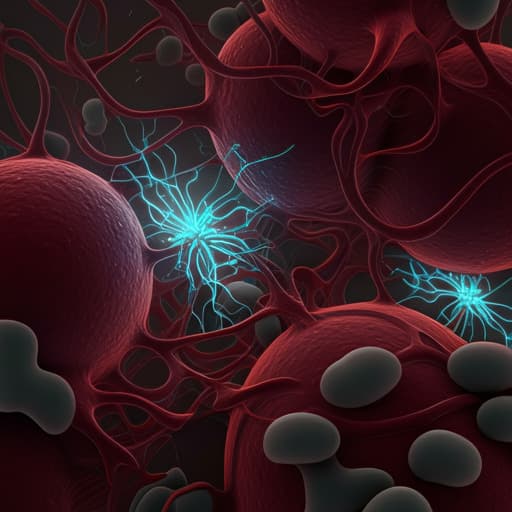
Sustained Cytotoxic Response of Peripheral Blood Mononuclear Cells from Unvaccinated Individuals Admitted to the ICU Due to Critical COVID-19 Is Essential to Avoid a Fatal Outcome
G. Orsi, G. Casado-fernández, et al.
This pivotal study by Giovanni Orsi and colleagues reveals the crucial role of peripheral blood mononuclear cell cytotoxic activity in the grim reality of unvaccinated individuals facing critical COVID-19. Key findings highlight significant differences in immune responses between those who survive and those who do not, emphasizing the importance of immunomodulatory treatments for improving survival rates in ICU settings.
Related Publications
Explore these studies to deepen your understanding of the subject.







