Health and Fitness
Social vulnerability amplifies the disparate impact of mobility on COVID-19 transmissibility across the United States
B. Huang, Z. Huang, et al.
The COVID-19 pandemic produced profound global disruptions and disproportionately affected disadvantaged populations. Given SARS-CoV-2 transmission via contact, droplets, and aerosols, human mobility is critical for spatial and temporal spread. However, how social vulnerability moderates the relationship between mobility and transmission remains underexplored. Prior work shows mobility reductions (e.g., stay-at-home orders, closures, travel restrictions) mitigated spread, but heterogeneous socioeconomic contexts question the appropriateness of applying uniform mobility–transmission relationships. Social vulnerability is multidimensional, involving interactions among social, natural, and engineered systems, and composite indices such as SoVI are often used. Existing studies often focus on single variables (e.g., income, age), neglecting combined effects. This study develops a composite COVID-19 Pandemic Vulnerability Index (CPVI) for US counties using PCA, extends SoVI dimensions with health and environmental factors, and evaluates how CPVI moderates the effects of intra- and inter-county mobility on COVID-19 transmissibility (Rt) during June–August 2020.
Extensive literature links mobility to COVID-19 spread using aggregated mobile phone data across spatial scales (e.g., Wuhan, US states and counties). Mobility restrictions served as key NPIs, with many countries implementing policies that reduced transmission. However, few studies directly examine how social vulnerability moderates the mobility–transmission association. Prior work explored associations between vulnerability and mobility or outcomes (e.g., income-related mobility reduction, infection risk by income, age structure with infection/mortality), but not heterogeneous mobility impacts across vulnerability groups. Social vulnerability is multidimensional; composite indices like SoVI summarize multiple factors. COVID-19-specific vulnerability indices have been developed using frameworks akin to social vulnerability or machine learning methods (e.g., random forest), each with trade-offs between predictive flexibility and theoretical interpretability. The gap identified is a comprehensive, theory-grounded index capturing multiple vulnerability dimensions to assess heterogeneous mobility effects on transmissibility.
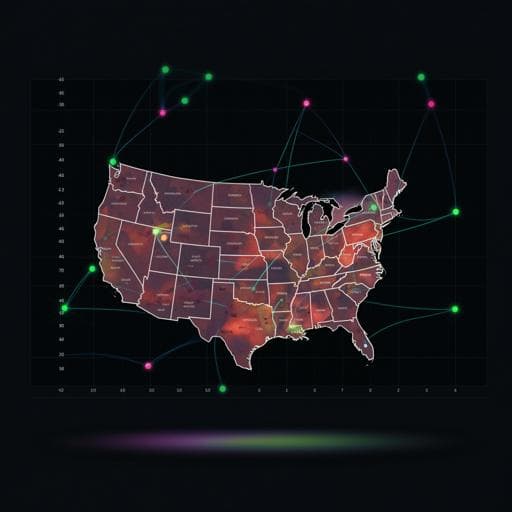
Data and period: COVID-19 daily confirmed cases and cumulative deaths for US counties were obtained from USAFacts (used by US CDC) from January 22 to September 1, 2020; daily new cases were derived. The analytical period for mobility–transmissibility relationships was June 1–August 31, 2020, after initial lockdowns and during reopening, focusing on a vaccine-free wave. County selection included contiguous US counties (excluding Alaska and Hawaii) with at least one case by June 1, 2020, and an average of at least three daily cases during June–August, yielding analysis counties (covering the majority of US population and cases during the period). Rt was computed for counties with sufficient incidence across 92 days, totaling 102,586 county-days (1,115 counties × 92 days).
County attributes for CPVI: Demographics and socioeconomics (elderly %, ethnic minority %, gender, language, education, income, poverty, unemployment), diseases (smoking, diabetes, hypertension, coronary heart disease), and health insurance from CDC 2015–2018; air pollution (annual PM2.5) from County Health Rankings & Roadmaps; medical capacity (air ambulance isolation rooms, hospital beds) from Area Health Resources Files; green space via NDVI (MODIS MOD13A2, averaged for 2019 using Google Earth Engine). Variables reflect factors associated with epidemic spread.
Mobility data and measures: SafeGraph provided daily county-level origin–destination (O-D) flows for January 1–September 1, 2020. For each county-day t, inflow, outflow, and internal (within-county) flows were computed. Baseline mobility was the average from January 1–21, 2020. Intracounty mobility ratio (IntraM_t) was defined as IntraFlow_t / IntraFlow_baseline; intercounty mobility ratio (InterM_t) as (Inflow_t + Outflow_t) / (Inflow_baseline + Outflow_baseline). Values >1 denote increases relative to baseline; <1 decreases. Mobility series were sometimes visualized with 7-day moving averages.
CPVI construction via PCA: Based on SoVI framework plus epidemiological and healthcare factors, variables included SoVI-related (elderly, ethnicity, gender, language, lower education attainment, income, poverty, unemployment) and health/environment/healthcare (smoking, diabetes, coronary heart disease, hypertension, air pollution, green exposure, isolation rooms, hospital beds, insurance). PCA with varimax rotation retained components with eigenvalues >1. Four principal components explained >70% variance: PC1 (38.58%: unemployment, poverty, ethnicity, elderly, lower education, language, groups—positive loadings), PC2 (16.63%: positive loadings for air pollution, hypertension, CHD, diabetes, smoking; negative for green exposure), PC3 (11.79%: negative for income, positive for insurance), PC4 (8.30%: negative for isolation rooms and hospital beds). Component scores were standardized (log-transform where necessary), directionality aligned with increased COVID-19 vulnerability, and combined using contribution weights to form CPVI. Counties were divided into quintiles (1=least vulnerable, 5=most vulnerable).
Rt estimation: Rt (effective reproduction number) was estimated using a Bayesian approach (Bettencourt & Ribeiro, 2008). Daily new cases inform Rt via likelihood P(k|Rt) with Poisson assumption for counts; serial interval assumed mean 7.5 days (SD 3.4). The method updates P(Rt|k) ∝ P(k|Rt)P(Rt), with λ linked to Rt via λ = k · L · (Rt − 1), where L is reciprocal of serial interval; priors and daily updates yield county-day Rt estimates.
Statistical modeling: A county fixed-effects model estimated the association between mobility and Rt, including interaction terms with vulnerability: Rt_it = β0 + β1 IntraM_it + β2 InterM_it + β3 CPVI_i + β4 (IntraM_it × CPVI_i) + β5 (InterM_it × CPVI_i) + Z_i + μ_it. Time-invariant county heterogeneity was absorbed via fixed effects; alternative specifications with time effects were also tested in robustness checks. Models were stratified by CPVI quintiles to estimate heterogeneous coefficients, and ANOVA contrasts assessed coefficient differences across vulnerability levels.
- Spatial and temporal transmissibility: Rt ≥ 1 counties peaked on July 1, 2020 (559 counties, >50% of studied counties), concentrated in California, Florida, and east-central states; fewer high-Rt counties by August 31.
- High transmissibility days by vulnerability: Percentage of county-days with Rt ≥ 1 increased with CPVI level. Totals across June–August: level 1=21.90%, level 2=28.19%, level 3=36.30%, level 4=39.93%, level 5=45.02%. Monthly: June (21.73, 29.10, 39.37, 43.38, 53.66%), July (30.74, 39.90, 49.15, 54.41, 58.72%), August (13.22, 15.62, 16.69, 22.11, 22.96%).
- Mobility recovery by vulnerability: During lockdown, more vulnerable counties exhibited larger mobility reductions and lower recovery. Intracounty mobility decreased by 24.94% (least vulnerable) vs 32.98% (most vulnerable), an 8.04% larger reduction for the most vulnerable. Intercounty mobility decreased by 62.72% (least vulnerable) vs 66.36% (most vulnerable), 3.64% larger reduction for the most vulnerable; pre-lockdown, more vulnerable counties had higher InterM, but during/after lockdown the trend reversed.
- Correlations between mobility and high transmissibility days: Across all counties, Pearson r for IntraM=0.53 and InterM=0.55 (p<0.05). By vulnerability level, IntraM correlation increased with vulnerability (r from 0.17 at level 1 to 0.68 at level 5; all p<0.05). InterM correlation rose to level 2 then stabilized (e.g., level 2 r≈0.63; level 5 r≈0.58; all p<0.05).
- Fixed-effects coefficients (Table 3): IntraM and InterM were positively associated with Rt across all levels (p<0.05). Coefficients (IntraM/InterM): level 1: 0.07/0.099; level 2: 0.19/0.12; level 3: 0.29/0.18; level 4: 0.22/0.28; level 5: 0.61/0.22. In the most vulnerable counties (level 5), IntraM’s effect was ~2× InterM’s.
- Marginal effects of 25% mobility change on Rt (Table 4): IntraM—level 1: 1.81% (IQR 1.01–3.15), level 2: 4.80% (2.89–6.72), level 3: 7.25% (3.59–9.06), level 4: 5.40% (3.52–7.27), level 5: 15.28% (13.35–17.21). InterM—level 1: 2.31% (1.83–2.79), level 2: 2.87% (2.36–3.39), level 3: 4.34% (3.63–5.03), level 4: 6.98% (6.23–7.72), level 5: 5.28% (4.48–6.08). Abstract highlight: level 5 IntraM effect (15.28%) is ~8× level 1 (1.81%).
- Heterogeneity tests (ANOVA contrasts, Table 5): For IntraM, coefficients formed three statistically distinct groups: level 1; levels 2–4; level 5 (p<0.05). For InterM, coefficients exhibited an inverted-U pattern: increasing significantly from levels 1–4 and decreasing at level 5; levels 1–2 were marginally different but both differed significantly from levels 3–5. Overall, mobility increased Rt at all vulnerability levels, but effects were substantially stronger in more vulnerable counties, especially for intracounty mobility.
The study demonstrates that social vulnerability, as captured by the CPVI, amplifies the impact of mobility on COVID-19 transmissibility. Counties with higher vulnerability experienced more days with Rt ≥ 1 and stronger mobility–Rt associations. Notably, intracounty mobility had a particularly strong effect in the most vulnerable counties, likely reflecting more frequent within-county contacts (e.g., households, local workplaces) relative to intercounty interactions. These findings address the research question by evidencing heterogeneous mobility effects conditioned by social vulnerability, implying that uniform mobility policies are suboptimal. Policy implications include tailoring social distancing and reopening strategies by vulnerability: prioritize reopening in low-vulnerability areas (levels 1–2), enforce stricter within-county mobility reductions and provide greater support in high-vulnerability areas (especially level 5). The observed reversal in relative mobility across vulnerability groups pre- vs post-lockdown highlights the importance of carefully defining mobility metrics (relative vs absolute) in policy evaluation and accounting for how restrictions may disproportionately affect vulnerable populations’ non-work mobility.
This study develops a comprehensive COVID-19 Pandemic Vulnerability Index (CPVI) integrating sociodemographic, environmental, epidemiological, and healthcare factors via PCA, and quantifies how social vulnerability moderates the relationship between mobility and COVID-19 transmissibility (Rt) across US counties during June–August 2020. Mobility increases Rt across all vulnerability levels, with substantially stronger effects in more vulnerable counties, particularly for intracounty mobility. The CPVI effectively captures communities bearing the greatest pandemic burden and supports targeted, vulnerability-informed interventions. Future work should refine vulnerability measurement (e.g., explore nonlinear feature relationships with kernel PCA or other methods), incorporate dynamic behavioral and policy variables, assess post-vaccination dynamics, and guide equitable allocation of interventions and vaccines considering environmental and healthcare capacity factors alongside age.
- Coverage and sample: Analysis was limited to a subset of US counties with sufficient incidence to estimate Rt during June–August 2020 (e.g., 1,115 counties in main analyses); results may not generalize to all counties. A limitation paragraph notes restricted coverage and potential inconsistencies in counts.
- Confounding and model specification: Time-invariant confounders were controlled via county fixed effects, but some observables (e.g., external temperature, public knowledge) and time-varying factors not captured uniformly across counties may remain. Robustness checks adding time fixed effects yielded consistent but magnified coefficients.
- Incubation/lag assumptions: Rt estimation and modeling assumed a serial interval (mean 7.5 days) and examined robustness to a 5-day incubation lag; interaction effects of CPVI and mobility were robust across tested lags.
- Behavioral factors: Preventive behaviors (e.g., mask wearing, avoidance of crowded places) likely affect both mobility and transmission; these were treated as relatively time-invariant during March–June and not explicitly modeled, potentially biasing estimates.
- PCA assumptions: Traditional (linear) PCA may not capture complex nonlinear relationships among vulnerability features; alternative methods (e.g., kernel PCA) could be explored.
- Policy/vaccination context: Analyses reflect a pre-vaccination period; subsequent interventions and vaccination campaigns may alter mobility–transmissibility relationships. Nonetheless, the framework remains applicable, with implications for prioritizing vaccine distribution based on broader vulnerability factors (e.g., air quality, green space, medical capacity).
Related Publications
Explore these studies to deepen your understanding of the subject.