Biology
Single-cell RNA sequencing reveals shared and distinct immune responses in Kawasaki disease and COVID-19
X. Liu, T. Luo, et al.
COVID-19 has persisted globally with significant cardiovascular complications. SARS-CoV-2 S protein can induce endothelial dysfunction, supporting a vasculitic component. Pediatric MIS-C shares features with KD, including cardiovascular involvement. KD is a leading cause of pediatric vasculitis with risk of coronary artery lesions (CAL), but mechanisms remain unclear. Given KD-like manifestations in COVID-19, elucidating shared inflammatory vascular injury mechanisms is critical. Interactions between PBMCs and vascular endothelial cells may drive coronary injury. This study used scRNA-seq of PBMCs from KD, COVID-19, and influenza cohorts, with experimental validation, to define immune mechanisms mediating endothelial injury and to discriminate shared versus disease-specific pathways.
Prior studies have implicated endothelial dysfunction in COVID-19 and recognized MIS-C as KD-like with cardiovascular involvement. Bulk transcriptomics in KD revealed immune activation but lacked cell-type resolution. scRNA-seq in KD identified altered monocyte subsets and poor differentiation of CD14 to CD16 monocytes, and broader immune alterations before/after IVIG, including changes in B and T cells. COVID-19 immunopathology studies underscored type I interferon pathways and monocyte involvement, with evidence that COVID-19 is a vasculitic disease affecting multiple organs. However, shared cellular and molecular mechanisms of vascular injury between KD and COVID-19, and functional validation, remained to be defined.
Study cohorts: Six children with complete KD (per AHA criteria) and three age-matched controls (KHC) were recruited (exclusions: cardiovascular malformations, prior autoimmune disease, monoclonal antibody therapy, hematologic diseases). Ethics approval and consent obtained. Public scRNA-seq PBMC datasets reanalyzed: 6 COVID-19 patients and 4 healthy adult controls (GSE150728), 3 influenza patients (GSE149689). Sample processing: 2 mL peripheral blood per subject; PBMCs processed for Chromium Single Cell 5' v2 (10x Genomics) library prep. Sequencing data processed with Cell Ranger v4.0.0. Quality control: Doublets removed using Scrublet (v0.2.3). Seurat v4 used to create objects; cells filtered (retain >1000 and <15000 UMIs; <20% mitochondrial reads). Samples with <500 or >5000 cells removed. Preprocessing/annotation: NormalizeData/ScaleData (Seurat). Batch correction and integration, dimensionality reduction (PCA/UMAP), neighbor graph and clustering with Azimuth; annotations verified by canonical markers. Cell-type prioritization with Augur (AUC scoring) comparing KD vs KHC and COV vs CHC. Pseudo-bulk analysis: DESeq2 used to identify DEGs (adjusted p<0.05, |log2FC|>1); normalized pseudo-bulk matrices analyzed by PCA (FactoMineR) and UMAP. Module scoring: AddModuleScore (Seurat) computed gene program scores (e.g., shared CD14 DEGs, IFN/ISM, M1/M2, adhesion profiles). Differential expression: FindMarkers (Seurat) with default params; DEGs required avg log2FC>0.25 and adjusted p<0.05. GO enrichment: clusterProfiler (enrichGO/compareCluster), visualization with ggplot2. In vitro experiments: Cell culture of HUVEC (DMEM) and THP-1 (RPMI 1640) at 37°C, 5% CO2. THP-1 transfections with siRNA (RNAiMAX); target genes: CCR1, DYSF, SELL, LMNB1, XAF1. RT-qPCR: RNA extracted (NucleoZOL), cDNA synthesized (PrimeScript RT with gDNA Eraser); qPCR (TB Green, Bio-Rad CFX96); normalized to 18S; 2^-ΔΔCt. Monocyte adhesion assay: Calcein AM-labeled, gene-silenced THP-1 cells incubated on HUVEC monolayers; nonadherent cells washed; adherent cells imaged and counted. Flow cytometry: PBMCs isolated; stained with anti-CD14, CD16, TLR4, CCR1, SELL; intracellular Lamin B1; measured on BD FACSCelesta, analyzed with FlowJo. Immunofluorescence: PBMC smears stained for CD14, DYSF, XAF1; DAPI nuclei; imaging on Olympus FV3000; quantification of double-positive cells. Coronary artery sections (KD vs donor) stained for CDH5 and γH2AX to assess endothelial injury. Statistics: R 4.1.0; Wilcoxon rank-sum with Bonferroni adjustment for multiple groups; chi-square/Fisher's exact for categorical; significance thresholds: *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001.
- Cell composition shifts: Elevated fraction of CD14+ classical monocytes in both KD and COVID-19 (p<0.05). Intermediate monocytes detected predominantly in KD; CD16+ non-classical monocytes showed no consistent change. Intermediate B cells reduced in KD and COV; plasmablasts increased, especially in COV; NK cells decreased in COV; MAIT cells reduced in COV and FLU.
- Cell-type responsiveness: Highest fractions of DEGs in classical monocytes in both KD and COV. Augur AUC indicated intermediate monocytes and Tregs highly responsive in KD vs KHC (AUC>0.9) but among least affected in COV vs CHC (AUC<0.6).
- Monocyte transcriptional programs: Over half of upregulated DEGs in KD CD14 monocytes (143/236; 60.59%) were shared with COV (not FLU). CD16 monocytes showed similarity between COV and FLU with more upregulated DEGs (153 vs 37). IFN and ISM scores were elevated in KD and COV classical monocytes. CD14 monocytes in FLU skewed toward M1 profile; KD/COV toward M2 markers (ARG1, CD163, MRC1, TGFB1), linked to endothelial dysfunction. IL-1β signaling genes were sparsely upregulated in KD/FLU and nearly absent in COV, suggesting IL-1β not central to shared vascular lesions.
- Endothelial vs epithelial adhesion profiles: CD14 monocytes in KD and COV showed increased endothelial adhesion gene profiles; CD16 monocytes in COV/FLU showed elevated epithelial adhesion profiles, aligning with cardiovascular vs pulmonary involvement.
- Candidate mediators: Five genes enriched in CD14 monocytes of KD/COV—SELL, CCR1, DYSF, LMNB1, XAF1—implicated in adhesion (SELL, CCR1), trafficking (LMNB1), and damage/apoptosis (DYSF, XAF1). Triple-positive SELL+/CCR1+/XAF1+ CD14 monocytes were significantly enriched in KD and COV compared with controls and FLU, and more specific than SELL+/CCR1+/LMNB1+.
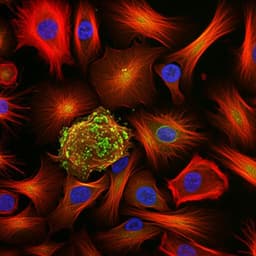
- Tissue evidence: KD coronary artery sections had more γH2AX+ endothelial cells (CDH5+), indicating endothelial injury.
- Functional validation: In THP-1–HUVEC assays, siRNA knockdown of CCR1, SELL, XAF1 reduced monocyte adhesion; knockdown of CCR1, SELL, LMNB1 reduced HUVEC IL6; all five knockdowns reduced TNF-α; SELL, LMNB1, XAF1 knockdown lowered HUVEC γH2AX+ cells. Combined knockdown of SELL/CCR1/XAF1 further decreased adhesion, IL6/TNF-α, and DNA damage.
- B cells: COV B-cell compartment dominated by plasmablasts; KD and FLU had higher naïve B fractions; memory B decreased in KD. GO terms showed type I IFN signaling enriched across B-cell subsets in KD/COV; COV uniquely enriched for antiviral responses in plasmablasts and intermediate B. Marker genes BST2, PSMB8, XAF1 high in KD/COV; PTPN6, IFITM2 mainly in KD.
- T cells: NK cells reduced in COV; KD exhibited activation signatures in NK and CD8 TEM (TCR gene expression). GO analyses showed "response to virus" in KD/COV CD8 TEM; only KD enriched "cellular response to interleukin-1" in CD8 TEM and "NF-κB transcription factor activity" in NK cells (KD-specific S100A8/A9/A12 vs COV CX3CR1).
The study delineates how innate immune activation—particularly of CD14+ monocytes—contributes to endothelial dysfunction common to KD and COVID-19, addressing the central question of shared vasculitic mechanisms. Shared IFN-driven programs and enrichment of SELL/CCR1/XAF1 triple-positive CD14 monocytes support a model in which monocyte adhesion and downstream endothelial damage drive CAL in KD and vascular injury in COVID-19. Conversely, CD16 monocyte programs associate with epithelial adhesion in COVID-19/FLU, aligning with pulmonary pathology in these diseases and highlighting COVID-19's dual vascular-respiratory involvement. Adaptive immune responses diverged: KD showed stronger activation of NK and CD8 TEM pathways (including interleukin-1 and NF-κB-related processes), while COV displayed marked plasmablast expansion and reduced NK cells. Functional assays confirmed that CCR1, SELL, and XAF1 promote monocyte–endothelial adhesion and inflammatory injury, nominating them as therapeutic targets. Limited IL-1β signaling overlap suggests previously proposed IL-1β pathways may not underpin shared KD/COVID-19 vascular lesions. Integrating scRNA-seq with in vitro validation strengthens causal inferences regarding monocyte-mediated endothelial injury.
Innate immune responses, particularly CD14+ monocyte activation, regulate endothelial dysfunction shared by KD and COVID-19, while adaptive immunity differs between diseases. COVID-19 monocytes exhibit adhesion to both endothelial and alveolar epithelial cells, explaining overlapping cardiovascular and respiratory phenotypes. CCR1, SELL, and XAF1 on CD14 monocytes emerged as potential therapeutic targets to mitigate endothelial injury in both KD and COVID-19.
- Lack of coronary artery tissue from COVID-19 patients for direct comparison.
- Small sample size (6 KD, 3 KHC; public datasets: 6 COV, 3 FLU, 4 CHC), potentially impacting statistical power and introducing variability.
- In vitro validation used THP-1 and HUVEC cell lines, which may not fully recapitulate in vivo monocyte–endothelium interactions.
- Heterogeneity and potential inconsistencies in publicly sourced datasets and batch effects despite integration methods.
Related Publications
Explore these studies to deepen your understanding of the subject.