Medicine and Health
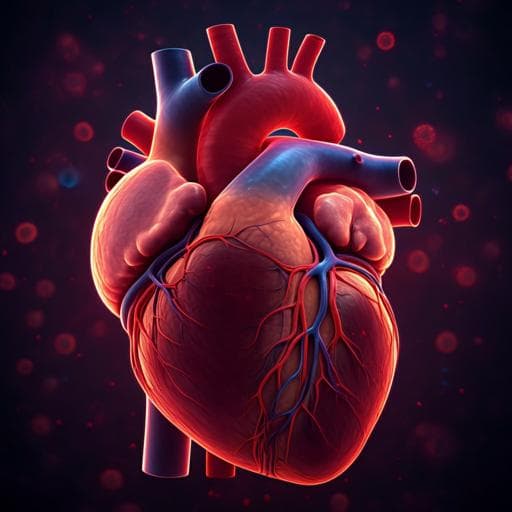
Self-assembling human heart organoids for the modeling of cardiac development and congenital heart disease
Y. R. Lewis-israeli, A. H. Wasserman, et al.
Cardiovascular disorders, including congenital heart defects (CHD), are leading causes of mortality and morbidity, yet in vitro human heart models have lagged behind other organ systems. Human pluripotent stem cells (hPSCs) can generate cardiac lineages, but conventional models lack 3D structure, extracellular matrix, and multicellular interactions, often omitting critical cell types such as epicardial and endocardial cells. Tissue-engineered cardiac constructs provide control but are costly, labor-intensive, and may not reflect native cell composition and organization. Recent self-assembling organoid approaches in mouse and human have begun to recapitulate early cardiogenesis but often rely on complex growth factor cocktails, co-cultures, or separate differentiation protocols. The authors aim to bridge this gap by developing a defined, reproducible, and scalable small-molecule-driven protocol to generate self-assembling human heart organoids (hHOs) that model cardiac development and can be used to study disease, including pregestational diabetes-induced CHD.
Prior work includes engineered cardiac tissues and cardiospheres that yield functional but structurally limited constructs and may use non-cardiac fibroblasts or HUVECs, reducing physiological relevance. Mouse ESC-derived precardiac organoids demonstrated heart field specification and cardiac crescent-like structures but are limited by species differences. Human cardioids with internal chambers have been reported, relying on complex growth factor mixtures, co-culture for epicardium, and independent protocols. Differentiation via canonical Wnt signaling modulation (activation/inhibition) is well established for cardiomyocytes, and morphogens BMP4 and Activin A are key in embryonic cardiac mesoderm patterning. Epicardial differentiation from PSCs has been achieved under defined conditions. These works motivate a streamlined, small-molecule-centric, self-assembling human heart organoid system with intrinsic multicell lineage complexity.
Human PSC lines (multiple iPSC lines and ESC H9) were maintained in Essential 8 Flex medium on Matrigel. For organoid generation, dissociated hPSCs were aggregated into embryoid bodies (EBs) by seeding 10,000 cells per well in round-bottom ultra-low attachment 96-well plates, centrifuging, and incubating for 48 hours (day −2 to day 0). A three-step Wnt signaling modulation protocol was applied: (1) Day 0 mesoderm induction with CHIR99021 (canonical Wnt activator via GSK3 inhibition), optimized at 1–4 µM; standard condition used 4 µM for 24 h. In some experiments, BMP4 (1.25 ng/ml) and Activin A (1 ng/ml) were added concurrently for 24 h. (2) Wnt inhibition with Wnt-C59 (PORCN inhibitor) at 2 µM from day 2 for 48 h (days 2–4). Media changes were performed by removing two-thirds of medium and replacing with fresh to minimize disturbance. Insulin-free RPMI/B27 was used until day 6, then RPMI/B27 with insulin from day 6 onward. (3) A second brief Wnt activation to induce proepicardial specification on day 7: CHIR99021 at 2 µM for 1 hour. Organoids were maintained with medium changes every 48 h and analyzed through day 19 and beyond. Beating onset occurred as early as day 6, robust by day 10, continuing at least 8 weeks. Optimization: CHIR99021 concentrations at day 0 (1, 2, 4, 6.6, 8 µM) were tested; 4 µM yielded maximal TNNT2+ content (~64.9% at day 15) and best function, likely aided by endogenous morphogen production under 3D conditions. For the second CHIR exposure (day 7), concentrations (2–8 µM) and durations (1–48 h) were tested; a single 1 h exposure at 2 µM produced physiologically relevant epicardial-to-myocardial ratios without overexpansion of epicardium. Disease modeling: Pregestational diabetes conditions were simulated by culturing organoids with RPMI containing 11.1 mM glucose and 1.14 nM insulin (PGDHOs) versus normoglycemic controls with 3.5 mM glucose and 170 pM insulin (NHOs). From day 7, oleate-BSA (40.5 µM), linoleate-BSA (22.5 µM), and 1-carnitine (120 µM) were added to enhance fatty acid metabolism. Assays and analyses: Immunofluorescence for cardiac lineages (cardiomyocytes TNNT2; epicardium WT1, TJP1; endocardium NFATc1; endothelium PECAM1; fibroblasts THY1, Vimentin). Confocal microscopy and quantitative image analysis across multiple z-planes with DAPI normalization. Bulk RNA-seq time course at days 0–19; alignment to hg38 (HISAT2), featureCounts, EdgeR differential expression; pathway enrichment and clustering; comparisons to monolayer differentiation and human fetal heart datasets (GSE106690); data deposited (GSE153185). Optical coherence tomography (custom SD-OCT) for 3D chamber topology. Transmission electron microscopy for ultrastructure. Electrophysiology using a custom 32-channel MEA to record organoid action potentials; analysis via Matlab Chronux toolbox. Calcium transient imaging using GCaMP6f iPSC line with 10 fps acquisition; ΔF/F0 computed after baseline correction. Seahorse assays (OCR, ECAR) on dissociated organoid cells with viability >90%. FlipGFP apoptosis reporter line used to assess programmed cell death. Statistical analyses used t-tests, one-way or two-way ANOVA with appropriate corrections; data presented as mean ± s.d. from at least 3 independent experiments unless specified.
- Three-step Wnt modulation in 3D EBs yields self-assembling human heart organoids (hHOs) with robust growth and beating as early as day 6; regular beating by day 10 and sustained for at least 8 weeks.
- Optimal day 0 CHIR99021 concentration is lower than monolayers: 4 µM produced highest cardiomyocyte content, 64.9 ± 5.3% TNNT2+ cells at day 15, and best functional metrics; protocol reproducible across multiple iPSC and ESC lines.
- A brief second Wnt activation (day 7, 2 µM CHIR, 1 h) induced proepicardial/epicardial formation while maintaining myocardium, yielding ~60–65% cardiomyocytes and 10–20% epicardial cells localized appropriately near the surface.
- Bulk RNA-seq revealed three developmental stages (pluripotency/early mesoderm; early cardiac development; fetal maturation). hHOs showed gene expression profiles closer to human fetal hearts than monolayer methods, including enrichment of epicardial, endothelial, endocardial, fibroblast, conduction, contractile, calcium handling, metabolism, and cardiac ECM gene programs.
- Lineage composition by imaging quantification: ~58.8% cardiomyocytes, 15.61% epicardial cells, 13.82 ± 1.54% endocardial cells, 12.49 ± 1.01% cardiac fibroblasts, 1.63 ± 0.21% endothelial cells (intermixed within myocardium), with ECM proteins (collagen I/IV, fibronectin) present.
- Heart field and chamber specification: Distinct HAND1 (FHF) and HAND2 (SHF) domains; atrial (MYL7+) and ventricular (MYL2+) cardiomyocytes localized to different regions (~48% atrial, ~18% ventricular of total cells at day 15). Large interconnected chamber-like structures observed, lined by NFATc1+ endocardium.
- Structural and functional maturation: OCT revealed 4–6 interconnected internal chambers; chamber volumes from ~5.5e-4 to 1.3e-2 mm^3. FlipGFP assays indicated minimal apoptosis in controls. TEM showed sarcomeres, mitochondria, gap junctions, glycogen, lipid droplets, and T-tubule-like structures (WGA staining). MEA recordings displayed robust, regular action potential waves with QRS-, P-, and T-like features; calcium imaging showed strong periodic Ca2+ transients.
- BMP4 + Activin A added at day 0 with CHIR increased organoid diameter (~15%), chamber interconnectivity (~50% increase in interconnected chambers; p=0.041), and PECAM1+ endothelial cells (~160% increase; p=0.0023), without altering myocardial or epicardial percentages.
- Pregestational diabetes modeling: PGDHOs showed early morphological differences (reduced elongation/patterning), larger size by day 8–14 (consistent with macrosomia; significant increases with p-values down to <0.0001), arrhythmic electrophysiological events, decreased OCR and increased glycolysis, fewer mitochondria and more lipid droplets by TEM, reduced ventricular (MYL2+) regions and enlarged atrial (MYL7+) regions, and aberrant epicardial/myocardial organization (epicardium enclosed by myocardium), recapitulating CHD-associated structural and metabolic defects.
The study demonstrates that brief, temporally controlled Wnt signaling modulation in self-assembled 3D hPSC aggregates yields heart organoids that closely recapitulate human fetal cardiac development at transcriptomic, structural, cellular, and functional levels. Inclusion of epicardial, endocardial, endothelial, and fibroblast populations, appropriate spatial organization, and formation of interconnected endocardium-lined chambers address limitations of prior 2D and engineered 3D models. The similarity of hHOs to fetal heart transcriptomes emphasizes their developmental relevance, while functional readouts (MEA, Ca2+ imaging, OCT) confirm physiological activity. Adding BMP4/Activin A enhances vascularization and chamber connectivity, suggesting synergy with small-molecule Wnt modulation and closer mimicry of in vivo morphogen gradients. The model’s ability to reproduce hallmarks of pregestational diabetes-induced CHD (growth abnormalities, arrhythmia, metabolic reprogramming, structural defects) underscores its utility for studying congenital heart disease mechanisms and could enable high-content drug screening and therapeutic discovery. Together, these findings advance human cardiac organoid technology toward more faithful developmental and disease modeling.
The authors present a defined, reproducible, and scalable protocol to generate self-assembling human heart organoids with multicellular complexity and fetal-like structural and functional features, including epicardium, endocardium, vasculature, and interconnected chambers with atrioventricular specification. Compared with monolayer differentiation, hHOs more closely resemble fetal heart transcriptomes and ECM composition. The platform models metabolic disease impacts on cardiac development, exemplified by pregestational diabetes-induced CHD phenotypes, highlighting potential applications in disease mechanism studies and therapeutic screening. Future work should enhance long-term developmental fidelity, improve anatomical and morphological realism, and establish functional, perfusable vascular networks to extend physiological relevance and enable modeling of coronary pathologies.
- Long-term culture can lead to deviation from normal developmental trajectories, reducing relevance with time.
- Despite improved complexity, organoids still do not fully recapitulate human heart development compared with in vivo models (e.g., mouse), particularly regarding complete anatomical fidelity and maturation.
- The vascular structures formed require further characterization to determine maturity, connectivity, and functional similarity to coronary vasculature; lack of a fully functional vascular network limits nutrient/waste exchange and organoid size.
- Bulk RNA-seq and immunofluorescence may not fully capture cellular heterogeneity; single-cell and advanced 3D imaging are needed for deeper resolution.
Related Publications
Explore these studies to deepen your understanding of the subject.