Medicine and Health
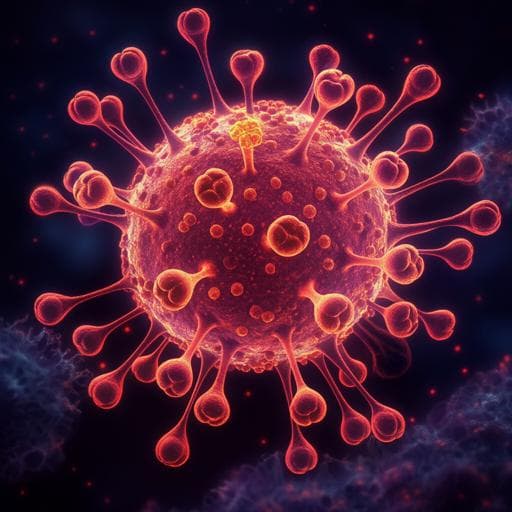
SARS-CoV-2 viral load is associated with increased disease severity and mortality
J. Faijnzlyber, J. Regan, et al.
This groundbreaking study reveals a strong connection between SARS-CoV-2 viral load and the risk of disease progression in COVID-19 patients. Conducted by a team of experts, it highlights how higher viral loads are linked to severe respiratory conditions and increased mortality, potentially aiding in patient risk stratification.
Related Publications
Explore these studies to deepen your understanding of the subject.