Medicine and Health
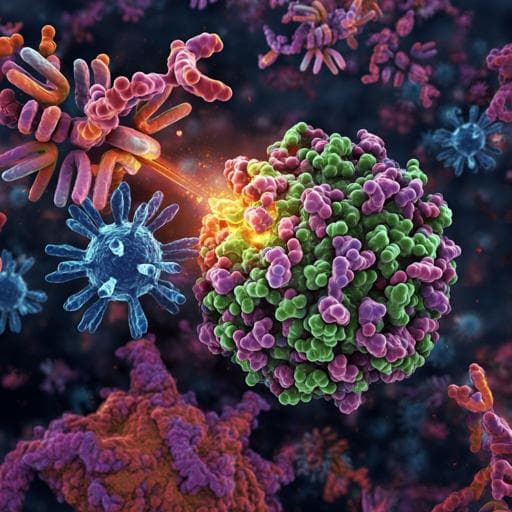
SARS-CoV-2 vaccination-infection pattern imprints and diversifies T cell differentiation and neutralizing response against Omicron subvariants
J. Wang, K. Li, et al.
Explore how different SARS-CoV-2 vaccination and infection histories affect immune responses to Omicron subvariants. Research conducted by Junxiang Wang, Kaiyi Li, Xinyue Mei, Jinping Cao, Jiaying Zhong, Peiyu Huang, Qi Luo, Guichang Li, Rui Wei, Nanshan Zhong, Zhu Xiang Zhao, and Zhongfang Wang reveals that Omicron infections generate stronger immune reactions compared to Delta, paving the way for improved vaccination strategies.
Related Publications
Explore these studies to deepen your understanding of the subject.