Medicine and Health
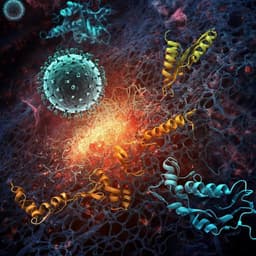
SARS-CoV-2 spike-protein D614G mutation increases virion spike density and infectivity
L. Zhang, C. B. Jackson, et al.
Discover the groundbreaking findings of how the SARS-CoV-2 spike protein D614G mutation significantly enhances viral entry into ACE2-expressing cells, thanks to the efforts of Lizhou Zhang and colleagues. This pivotal study reveals how the mutated S protein incorporates more effectively into the virion, making it a dominant force in COVID-19 transmission.
Related Publications
Explore these studies to deepen your understanding of the subject.