Medicine and Health
Recent advances in immunotherapy and molecular targeted therapy for gastric cancer
Y. Yoshinami and H. Shoji
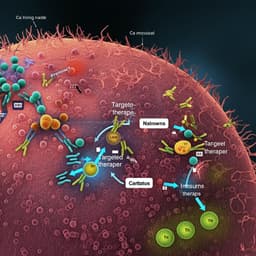
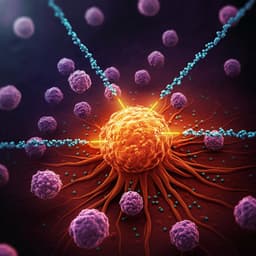
Gastric cancer is the fourth most common malignancy and a leading cause of cancer death worldwide. For advanced unresectable or recurrent disease (AGC), standard first-line regimens have historically included a fluoropyrimidine plus a platinum agent, with trastuzumab added in HER2-overexpressing tumors; second-line paclitaxel with or without ramucirumab is also standard. Despite these therapies, median survival remains approximately 12–15 months. The emergence of immune checkpoint inhibitors (ICIs), particularly PD-1/PD-L1 inhibitors, has provided new therapeutic opportunities: pembrolizumab is licensed for MSI-H/TMB-high tumors and, in combination with trastuzumab and chemotherapy, in first-line HER2-positive AGC; nivolumab has demonstrated survival benefit as third-line therapy in ATTRACTION-2 and, in combination with chemotherapy, as first-line therapy in CheckMate-649. Numerous clinical trials are evaluating combinations of ICIs with cytotoxics, other ICIs (e.g., CTLA-4), and targeted agents (e.g., anti-VEGF, HER2, CLDN18.2), as well as cellular therapies (CAR-T). This review summarizes molecular subtypes, biomarkers, and the current evidence base for immunotherapy and targeted therapies in AGC across treatment settings.
The review synthesizes data on the molecular taxonomy of gastric cancer (TCGA-defined subtypes: EBV-positive, MSI, chromosomal instability, and genomically stable) and their distinct immunologic profiles. EBV-positive and MSI-H/dMMR tumors show higher likelihood of response to PD-1 blockade; CIN tumors often exclude T cells and macrophages from the tumor microenvironment, suggesting strategies to modulate immunosuppression. The authors summarize pivotal and emerging clinical trials across lines of therapy: first-line PD-1 inhibitors plus chemotherapy (CheckMate-649, ATTRACTION-4, ORIENT-16, KEYNOTE-859, RATIONALE-305), maintenance strategies (JAVELIN Gastric 100), second-line pembrolizumab versus paclitaxel (KEYNOTE-061), and third- or later-line nivolumab (ATTRACTION-2) and pembrolizumab (KEYNOTE-059). Perioperative immunotherapy trials (NEONIPIGA, KEYNOTE-585, MATTERHORN, ATTRACTION-5) are reviewed. Biomarker-driven sections cover MSI-H/dMMR responses (KEYNOTE-158 and post-hoc analyses across KEYNOTE programs), TMB as an imperfect tumor-agnostic biomarker, and PD-L1 CPS as a stratifier for benefit. Combination approaches include PD-1 plus CTLA-4 (e.g., ATTRACTION-6; Moonlight), PD-1 plus multikinase/anti-VEGF agents (REGONIVO, EPOC1706, LEAP-015), PD-1 plus HER2-directed agents (KEYNOTE-811; trastuzumab deruxtecan programs; margetuximab; zanidatamab; tucatinib combinations), and PD-1 with CLDN18.2 targeting (zolbetuximab programs). Additional immuno-oncology targets (LAG-3, TIGIT), bispecific antibodies (including CLDN18.2 x CD3), and CLDN18.2-directed CAR-T therapies are discussed, outlining early efficacy signals and ongoing trials.
This is a narrative review of the contemporary literature and clinical trial data on immunotherapy and molecular targeted therapy for gastric cancer up to early 2023. The authors compile and discuss results from phase I–III clinical trials, biomarker analyses, and translational studies across treatment settings (first-line, second-line, third- or later-line, and perioperative). No formal systematic search strategy, inclusion/exclusion criteria, or meta-analytic methods are described.
- First-line PD-1 plus chemotherapy:
- CheckMate-649: Nivolumab + chemotherapy improved OS and PFS versus chemotherapy in PD-L1 CPS ≥5 (OS HR 0.71; PFS HR 0.68) with benefits extending to CPS ≥1 and the intent-to-treat population; median OS 14.4 vs 11.1 months at 24-month follow-up in CPS ≥5.
- ATTRACTION-4: Improved PFS with nivolumab + chemotherapy; OS not significantly different, potentially due to high post-progression therapy use.
- ORIENT-16: Sintilimab + chemotherapy improved OS in all randomized patients (median 15.2 vs 12.3 months; HR 0.77) and in CPS ≥5 (median 18.4 months; HR 0.66).
- KEYNOTE-859: Pembrolizumab + chemotherapy improved OS (12.9 vs 11.5 months; HR 0.78) and PFS (6.9 vs 5.6 months; HR 0.76) in the overall population.
- RATIONALE-305 (interim, PD-L1 positive): Tislelizumab + chemotherapy improved OS (17.2 vs 12.6 months; HR 0.74) and PFS (7.2 vs 5.9 months; HR 0.67).
- KEYNOTE-062: Pembrolizumab monotherapy non-inferior to chemotherapy in CPS ≥1; trend to OS benefit in CPS ≥10; combination arm did not significantly improve outcomes over chemotherapy.
- Second-line:
- KEYNOTE-061: Pembrolizumab did not significantly improve OS versus paclitaxel in CPS ≥1 overall; greater long-term benefit in select subgroups (ECOG 0, CPS ≥10, MSI-H).
- Third-/later-line:
- ATTRACTION-2: Nivolumab improved OS (5.26 vs 4.14 months; HR 0.63), PFS (HR ≥0.60), and ORR (11.2% vs 0%) versus placebo.
- KEYNOTE-059: Pembrolizumab ORR 11.6% overall (15.5% CPS ≥1; 6.4% CPS <1); median OS 5.6 months; safety consistent with PD-1 inhibitors.
- Perioperative:
- NEONIPIGA (localized dMMR/MSI-H): Neoadjuvant nivolumab + ipilimumab followed by adjuvant nivolumab achieved pathologic complete response rate ~58.6%.
- Biomarker-defined responses:
- MSI-H/dMMR across KEYNOTE-059/061/062 and KEYNOTE-158: High response rates and durable benefit; in KEYNOTE-061 MSI-H post-hoc, pembrolizumab median OS not reached vs 8.1 months with paclitaxel (HR 0.42).
- TMB-high: Pembrolizumab tumor-agnostic approval at ≥10 mut/Mb; threshold appropriateness in gastric cancer remains uncertain.
- EBV-positive AGC: Small studies show promising responses to PD-1/PD-L1 inhibitors, but evidence remains limited.
- Combination immunotherapy/targeted approaches:
- PD-1 + CTLA-4: Mixed results; toxicity considerations; exploratory benefit signals in some phase II designs (e.g., Moonlight).
- PD-1 + multikinase/anti-VEGF: REGONIVO (regorafenib + nivolumab) ORR 44%, median PFS 5.6 months, including responses after prior PD-1; lenvatinib + pembrolizumab ORR 69%, median PFS 7.1 months; LEAP-015 safety run-in ORR ~73% with chemo backbone.
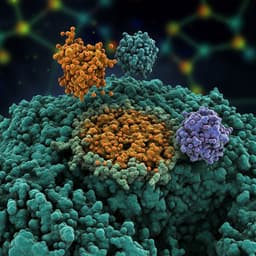
- PD-1 + HER2 targeting: KEYNOTE-811 showed ORR 77.4% vs 51.9% (+22.7% absolute) with pembrolizumab + trastuzumab + chemotherapy; more complete responses; T-DXd active post-trastuzumab (second-/later-line); margetuximab + PD-1 and zanidatamab combinations show promising activity; ongoing phase III programs.
- CLDN18.2 targeting: Zolbetuximab + chemotherapy improved outcomes in CLDN18.2-positive disease (phase II/III data); combinations with ICIs under study.
- Emerging checkpoints and modalities:
- LAG-3 and TIGIT inhibitors combined with PD-1/chemo are in clinical evaluation; early signals with vibostolimab + pembrolizumab.
- Bispecific antibodies (e.g., CLDN18.2 x CD3) and CLDN18.2-directed CAR-T cells show early activity; CLDN18.2 CAR-T ORR ~57.1% with acceptable tolerability.
Collectively, evidence supports PD-1 inhibitor plus chemotherapy as a standard first-line option for HER2-negative AGC across PD-L1 expression levels, with the greatest magnitude of benefit in CPS ≥5 populations. Biomarker selection refines treatment decisions: MSI-H/dMMR tumors derive substantial and durable benefit from PD-1 blockade across lines, while the utility of TMB thresholds in gastric cancer remains unresolved. Heterogeneity in outcomes, such as the lack of OS benefit in ATTRACTION-4, may be influenced by extensive post-progression treatments. In HER2-positive disease, adding PD-1 blockade to trastuzumab and chemotherapy significantly increases response rates, supporting incorporation into first-line care. Combination strategies targeting immunosuppressive pathways (VEGF axis, macrophage modulation) and dual-checkpoint blockade (PD-1 + CTLA-4) show potential to overcome resistance and broaden benefit, though toxicity and optimal sequencing require clarification. Perioperative immunotherapy demonstrates encouraging pathologic response rates, especially in dMMR/MSI-H disease, but remains investigational. Ongoing trials targeting LAG-3, TIGIT, CLDN18.2, and employing bispecific antibodies and CAR-T therapies reflect a rapidly evolving landscape aimed at enhancing efficacy and addressing primary and acquired resistance.
Immunotherapy has reshaped the treatment paradigm for advanced gastric cancer. First-line PD-1 inhibitor–chemotherapy combinations improve survival, and dual HER2–PD-1 targeting enhances response in HER2-positive disease. MSI-H/dMMR status identifies patients with high likelihood of durable benefit across settings. Promising results from combinations with multikinase inhibitors, additional checkpoints (CTLA-4, LAG-3, TIGIT), and antibody–drug conjugates (e.g., trastuzumab deruxtecan) suggest further gains are achievable. Perioperative use of ICIs shows high pathologic response in biomarker-selected patients but remains under investigation. Future priorities include refining biomarker-driven patient selection (PD-L1 CPS, MSI-H, emerging genomic/immunologic signatures), validating tumor-specific TMB thresholds, optimizing combination partners and sequencing, and monitoring long-term safety. Continued clinical research is expected to expand effective options and improve outcomes for gastric cancer.
As a narrative review, the article does not describe systematic search methods or formal bias assessment. Some cited trials are interim analyses or conference reports with immature OS data. Cross-trial comparisons are limited by differences in study populations, PD-L1 assays and CPS cutoffs, geographic treatment patterns (e.g., post-progression therapy access), and chemotherapy backbones. Evidence for certain subgroups (e.g., EBV-positive tumors) is based on small cohorts or case reports. The generalizability of tumor-agnostic TMB cutoffs to gastric cancer is uncertain, and perioperative immunotherapy data are preliminary.
Related Publications
Explore these studies to deepen your understanding of the subject.