Medicine and Health
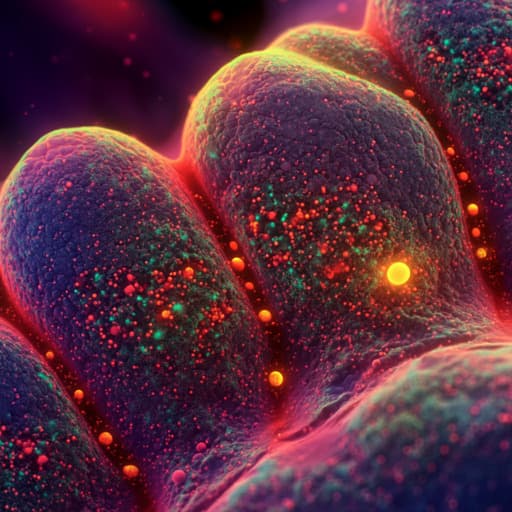
Real-time visualization of lung malignancy with needle-based confocal laser endomicroscopy during shape-sensing robotic-assisted bronchoscopy
F. Diaz-churion, A. Y. Lee-mateus, et al.
This groundbreaking case series explores the innovative combination of robotic-assisted bronchoscopy and needle-based confocal laser endomicroscopy, revealing high-resolution insights into solitary pulmonary nodules. Conducted by a team at the Mayo Clinic, this research confirms the presence of malignancy in all cases, showcasing a potential leap in diagnostic accuracy for pulmonary lesions.
Related Publications
Explore these studies to deepen your understanding of the subject.