Medicine and Health
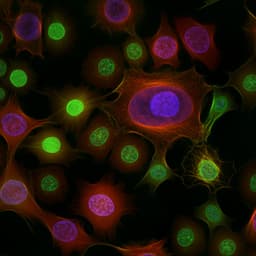
Potential Pathophysiological Pathways in the Complex Relationships between OSA and Cancer
M. Sánchez-de-la-torre, C. Cubillos, et al.
Discover the intriguing connection between obstructive sleep apnea and cancer incidence as explored by researchers Manuel Sánchez-De-La-Torre, Carolina Cubillos, Olivia J Veatch, Francisco Garcia-Rio, David Gozal, and Miguel Angel Martinez-Garcia. This study delves into how factors like hypoxemia and obesity may influence cancer risk, revealing vital pathophysiological pathways that warrant further investigation.
Related Publications
Explore these studies to deepen your understanding of the subject.