Medicine and Health
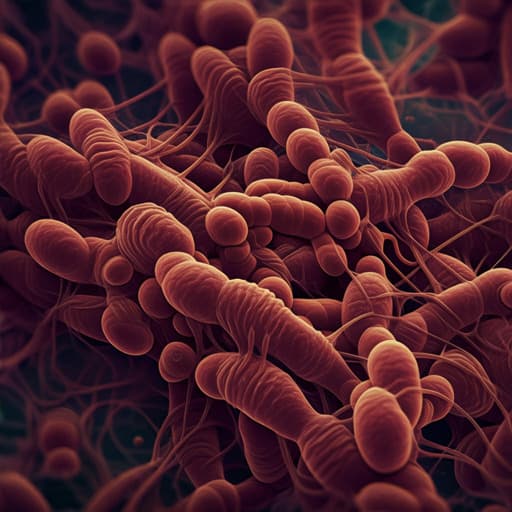
Parasites and childhood stunting -a mechanistic interplay with nutrition, anaemia, gut health, microbiota, and epigenetics
I. L. Gabain, A. S. Ramsteijn, et al.
Explore the intricate connections between parasitic infections and childhood stunting in this thought-provoking opinion paper by Isobel L Gabain, Anouschka S Ramsteijn, and Joanne P Webster. Delve into the mechanisms linking these issues, including malnutrition, environmental dysfunction, and gut health. Discover the urgent need for more research to untangle these complex relationships.
Related Publications
Explore these studies to deepen your understanding of the subject.