Medicine and Health
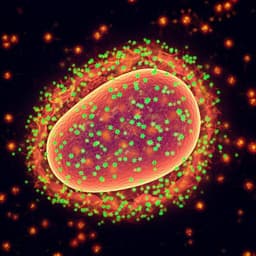
Off-the-shelf CAR natural killer cells secreting IL-15 target spike in treating COVID-19
T. Lu, R. Ma, et al.
The study addresses the need for targeted, rapidly deployable therapies for COVID-19, a global pandemic caused by SARS-CoV-2. Existing treatments such as remdesivir and dexamethasone have limitations, and while several monoclonal antibodies and oral antivirals have emergency authorization, no cellular immunotherapies are approved. Natural killer (NK) cells are innate lymphocytes capable of lysing virally infected and malignant cells, but they lack specificity for SARS-CoV-2. Because viral entry depends on binding of the spike protein (S1 subunit) to the ACE2 receptor on host cells, the authors hypothesized that engineering NK cells to express an ACE2-based CAR would provide specificity to target spike-expressing cells. To enhance NK cell persistence, the team co-expressed soluble IL-15. The research question is whether mACE2-CAR_sIL15 NK cells can specifically bind spike, exert enhanced cytotoxic and cytokine responses against spike-expressing targets, and protect against live SARS-CoV-2 infection in vivo, potentially providing an off-the-shelf cellular therapy.
The paper situates its work within the context of COVID-19 therapeutics, noting emergency approvals of remdesivir and dexamethasone with limited efficacy and lack of direct antiviral activity for steroids. Additional approvals include oral antivirals (Lagevrio and Paxlovid) and multiple monoclonal antibodies targeting SARS-CoV-2 for outpatient use. Prior work in CAR-NK therapy showed promising outcomes in lymphoid malignancies with CAR NK cells co-expressing IL-15. Structural studies established the role of the SARS-CoV-2 spike S1 subunit in ACE2 binding, and neutralizing antibodies targeting S1 can block infection. Clinical and immunologic observations indicate reduced NK and cytotoxic T-cell numbers and increased inhibitory/exhaustion markers (e.g., NKG2A, PD-1, Tim-3) in COVID-19 patients. These findings support exploring engineered NK cells endowed with specificity to spike and augmented persistence via IL-15.
- CAR design and cell engineering: A mutant extracellular domain of ACE2 (zinc metallopeptidase domain) was fused to IgG1 hinge and CD28 transmembrane/intracellular domains plus CD3ζ, and linked via T2A to truncated LNGFR (marker). A separate vector encoded human soluble IL-15 (signal peptide–codon-optimized IL-15–CSF2R signal peptide) followed by truncated EGFR (marker). Two retroviral vectors were produced in GP2-293 cells using Lipofectamine 2000.
- NK cell source and expansion: Primary human NK cells were isolated from umbilical cord blood (UCB) with IRB-approved consent. NKs were expanded for 5 days with K562 feeder cells expressing IL-1β and membrane-bound IL-21 (APC K562) in IL-2. Expanded NKs were retrovirally transduced with both vectors to generate mACE2-CAR_sIL15 NK cells. Expression of markers (LNGFR for CAR, EGFR for sIL15) was assessed by flow cytometry; FACS sorting enriched co-expressing cells.
- Phenotyping: Expression of activating/inhibitory receptors (e.g., CD16, CD69, NKp30/44/46, NKG2D, TRAIL, CD25, DNAM-1, CD62L, CD94, KIRs) was profiled and compared to control NKs transduced with EGFR only or sIL15 only.
- Binding assays: mACE2-CAR_sIL15 and control NK cells were incubated with His-tagged recombinant spike S1 protein and stained with anti-His for flow cytometry. Binding to VSV-SARS-CoV-2 chimeric viral particles was assessed using anti-spike primary and fluor-conjugated secondary antibodies by flow cytometry.
- Cytotoxicity and functional assays: Target cells were A549 human lung carcinoma cells stably expressing SARS-CoV-2 spike (A549-spike) or parental A549. Real-time cell analysis (RTCA) measured cytotoxicity at various E:T ratios. Degranulation (CD107a) and intracellular cytokines (TNF-α, IFN-γ) were measured after 4 h co-culture (E:T 4:1). IL-15 secretion was quantified by ELISA from 72 h supernatants of cultures with or without A549-spike.
- Cryopreservation studies: Post-thaw viability, CAR expression, and cytotoxicity against A549-spike were evaluated up to 6 h after thaw; comparisons were made to thawed control NKs.
- In vivo NSG xenograft: NSG mice received i.v. FFLuc-labeled A549-spike cells (day 0) and i.v. infusions (10×10^6/mouse) of vehicle, control tEGFR NK cells, control sIL15 NK cells, or mACE2-CAR_sIL15 NK cells on days 0, 2, and 4. Tumor burden was monitored by bioluminescent imaging on days 0, 6, 13, and 19; tissues were analyzed on day 20 for human NK presence and CAR expression.
- K18-hACE2 SARS-CoV-2 infection model: K18-hACE2 transgenic mice were immune-cell–depleted to prevent xenorejection, infected intranasally with live SARS-CoV-2 (1×10^3–1×10^4 PFU), and treated on day 1 with vehicle, control NKs, or mACE2-CAR_sIL15 NK cells. Body weight and survival were tracked. Viral RNA copy numbers (spike) in brain and lung were quantified by RT-qPCR; immunohistochemistry assessed nucleocapsid protein in tissues. Plasma cytokines (17-plex including IL-6, IL-10, IL-17A, IFN-γ, TNF-α, GM-CSF) were measured by Luminex at day 4 post-treatment.
- Statistics: Two-tailed t-tests for two-group comparisons; one-/two-way ANOVA with multiple-comparison adjustments (Holm–Sidak, Hochberg, Dunn) for multi-group analyses; Kaplan–Meier survival with Gehan–Breslow–Wilcoxon; significance at p<0.05.
- Successful generation of mACE2-CAR_sIL15 NK cells from UCB, with ~90% of FACS-sorted cells co-expressing CAR (LNGFR+) and sIL15 (EGFR+) after 14 days in vitro.
- Specific binding: CAR-positive mACE2-CAR_sIL15 NK cells bound recombinant spike S1 protein; no binding observed in CAR-negative subsets or control NKs. mACE2-CAR_sIL15 NK cells also bound VSV-SARS-CoV-2 chimeric viral particles.
- Enhanced cytotoxicity: In RTCA assays, mACE2-CAR_sIL15 NK cells showed significantly greater killing of A549-spike targets at multiple E:T ratios compared with control NKs, with no comparable increase against parental A549 cells.
- Increased effector function: Upon co-culture with A549-spike, mACE2-CAR_sIL15 NK cells exhibited elevated degranulation (CD107a) and cytokine production (TNF-α, IFN-γ) versus controls.
- IL-15 secretion: Engineered NK cells produced soluble IL-15 at a mean of 572.7 pg/mL per 10^6 cells (range 36.9–943.9 pg/mL per 10^6 cells), supporting persistence and function.
- Cryopreservation robustness: Post-thaw functional recovery exceeded 80% with >90% viability; CAR expression remained comparable to fresh cells. Viability remained >80% at 6 h post-thaw. Cryopreserved mACE2-CAR_sIL15 NK cells retained superior cytotoxicity against A549-spike compared to thawed control sIL15 NKs.
- NSG xenograft efficacy: Repeated infusions of mACE2-CAR_sIL15 NK cells improved control of A549-spike tumor growth relative to vehicle and control NK treatments. Human NK cells, including CAR-expressing cells, were detectable in blood, spleen, and liver at day 20, indicating persistence and homing.
- Protection in SARS-CoV-2 infection model: In K18-hACE2 mice infected with live virus, mACE2-CAR_sIL15 NK treatment mitigated weight loss, significantly improved survival (all vehicle died by day 6; control NKs by day 7; 60% of mACE2-CAR_sIL15–treated mice survived at least 12 days), and reduced viral RNA copies in brain and lung. Nucleocapsid protein staining was decreased in treated animals.
- Safety: Plasma cytokine levels (including IL-6, IL-10, IL-17A, IFN-γ, TNF-α, GM-CSF) did not differ significantly between mACE2-CAR_sIL15 NK–treated and control groups, suggesting low risk of cytokine-mediated toxicity.
The findings demonstrate that equipping NK cells with an ACE2-based CAR confers specific recognition of SARS-CoV-2 spike, translating into enhanced cytotoxicity and cytokine responses against spike-expressing targets. Co-expression of soluble IL-15 supports NK cell persistence and activity, addressing the inherently short in vivo lifespan of mature NK cells. Binding to both recombinant S1 and spike-bearing viral particles indicates target engagement relevant to infection. In vivo, the engineered NK cells reduced viral burden and improved survival in susceptible K18-hACE2 mice without elevating systemic cytokines, supporting a favorable safety profile. The two-vector strategy increased transduction efficiency at the cost of manufacturing complexity but enabled robust co-expression of CAR and sIL-15. The cryopreservation data support the development of an allogeneic, off-the-shelf product that retains activity after thawing, facilitating rapid deployment for high-risk patients with COVID-19. Collectively, the results support the therapeutic potential of mACE2-CAR_sIL15 NK cells as a targeted antiviral cellular therapy.
The study presents a novel off-the-shelf, cryopreservable mACE2-CAR_sIL15 NK cell therapy that specifically targets SARS-CoV-2 spike, shows potent in vitro and in vivo efficacy, reduces viral loads, improves survival in a transgenic mouse model, and maintains a favorable cytokine safety profile. The approach leverages abundant UCB resources for scalable manufacturing. Given the observed robustness after cryopreservation and efficacy in preclinical models, the product is a promising candidate for clinical testing in critically ill COVID-19 patients and may be applicable to other coronaviruses utilizing spike-ACE2 entry. Future work includes GMP manufacturing, clinical trials to assess safety and efficacy in humans, and evaluation against emerging variants and related coronaviruses.
The authors note the use of a two-vector system to co-express CAR and sIL-15, which increases transduction efficiency but necessitates separate vector manufacture and adds cost and complexity. Efficacy and safety were demonstrated in preclinical mouse models with immune-cell depletion to prevent xenorejection; clinical efficacy and safety in humans remain to be determined.
Related Publications
Explore these studies to deepen your understanding of the subject.