Medicine and Health
Non-antibiotic pharmaceuticals are toxic against *Escherichia coli* with no evolution of cross-resistance to antibiotics
R. J. Hall, A. E. Snaith, et al.
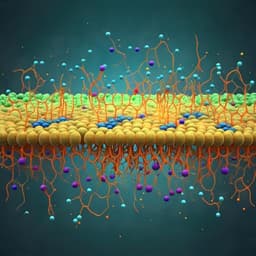
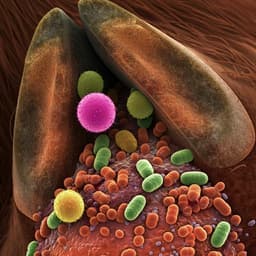
Antimicrobial resistance (AMR) is a major public health concern, and effluents from pharmaceutical production and wastewater treatment facilities contribute to AMR by releasing biologically active compounds into the environment. Beyond antibiotics, non-antibiotic pharmaceuticals (active ingredients and formulation components) are frequently detected in water bodies worldwide. While bacterial evolution in response to antibiotics is well characterized, the effects of prolonged exposure to non-antibiotic pharmaceuticals on bacterial growth, stress responses, genetic adaptation, and potential selection for cross-resistance to antibiotics remain unclear. This study investigates whether selected non-antibiotic pharmaceuticals at environmentally relevant concentrations exhibit intrinsic toxicity toward Escherichia coli K-12 MG1655, whether long-term exposure leads to genetic changes, and whether such exposure can co-select for cross-resistance to clinically relevant antibiotics.
Prior studies show species- and compound-specific antimicrobial activities of non-antibiotic pharmaceuticals; for example, certain vasodilators and norepinephrine reuptake inhibitors inhibit growth of E. coli, Staphylococcus aureus, Pseudomonas aeruginosa, and Candida albicans. A broad screen reported over 200 human-targeted drugs affecting at least one gut bacterial species, typically with narrow spectra. Titanium dioxide (TiO2), commonly used across industries, has demonstrated antibacterial effects against E. coli, P. aeruginosa, S. aureus, and Enterococcus faecalis, often studied as surface coatings rather than in suspension (the likely environmental exposure form). Non-antibiotic pharmaceuticals can modulate horizontal gene transfer: ibuprofen, diclofenac, propranolol, and carbamazepine have been associated with enhanced uptake or transfer of antibiotic resistance genes, potentially via increased competence, membrane permeability, or conjugation. Conversely, some drugs (e.g., metformin, benzydamine) can increase antibiotic uptake and resensitize multidrug-resistant pathogens, suggesting complex and context-dependent interactions. These findings motivate investigation into intrinsic toxicity, mechanisms of action, and the potential for non-antibiotic pharmaceuticals to act as selection pressures for cross-resistance to antibiotics under environmentally relevant exposures.
Organism and toxicity screening: Escherichia coli K-12 MG1655 was grown from glycerol stock to overnight culture in LB, diluted to OD600 ~0.5, and exposed to serial dilutions of acetaminophen, ibuprofen, propranolol, metformin, and titanium dioxide (TiO2 nanoparticles) at concentrations including environmentally relevant levels (see Supplementary Table 1). In 96-well plates, 99 µL LB + compound plus 1 µL diluted cells were incubated at 37 °C with shaking for 24 h; OD600 was measured every 30 min in triplicate. Area under the curve (AUC) was computed; significance assessed by one-way ANOVA.
Transcriptomics under ibuprofen: Triplicate cultures were grown in LB with or without 50 µg/mL ibuprofen (ethanol solvent control used). At OD600 ~0.9, cells were harvested, washed, and pellets frozen. RNA sequencing (GENEWIZ) was performed. Reads were quantified with Kallisto (v0.48.0) using a Prokka-annotated long-read assembly of the ancestor as reference; differential expression analyzed in Degust with FDR p < 0.05 and |log2FC| ≥ 1.
Selection experiment (long-term exposure): Six independent biological replicate populations per condition were propagated in nutrient broth (NB) with acetaminophen (5 ng/mL), ibuprofen (2 µg/mL), TiO2 (1 µg/mL), propranolol (0.5 ng/mL), metformin (0.5 ng/mL), or NB-only control. Daily 1% transfers were performed for 30 days at 37 °C with agitation. End-point populations were preserved; growth kinetics of evolved populations were assayed in the presence of the respective selection compound at 1× and 100× concentrations compared to the ancestral lineage. A 7-day recovery experiment (serial passage in NB without compounds) was conducted to test reversibility of compound effects.
Genome sequencing and analysis: Ancestral and evolved isolates underwent Illumina short-read sequencing (MicrobesNG) and Oxford Nanopore MinION long-read sequencing. Libraries: SQK-LSK109, EXP-NBD114; basecalling with Guppy v6.0.1; read filtering with Filtlong v0.2.1; demultiplexing with qcat v1.1.0. Hybrid assemblies were generated with Unicycler v0.4.8-beta (bold mode). Panaroo v1.2.10 produced gene presence/absence and core alignments; phylogeny constructed with IQ-TREE v2.2.0.3; visualized in Phandango. SNPs were called with Snippy v4.3.6. Insertion sequence (IS) elements were analyzed with ISEScan v1.7.2.3, ISFinder, and a custom ABRicate (v0.8) database; manual inspection in Unipro UGENE v47.0. Presence/variation of ldrA was assessed with a custom ABRicate database.
Antibiotic susceptibility testing: Minimum inhibitory concentrations (MICs) were determined in Iso-Sensitest Broth using standard microdilution for the MG1655 ancestor, an evolved isolate from ibuprofen exposure, and E. coli ATCC 25922 (quality control). Agents: ethidium bromide, ampicillin, ciprofloxacin, chloramphenicol, trimethoprim, colistin. Checkerboard assays measured combined effects of ibuprofen with each antimicrobial in MG1655 and ATCC 25922. Fractional inhibitory concentration (FIC) indices were calculated, with 0.5–4 indicating no synergy/antagonism. Results for ATCC 25922 were validated against expected ranges.
Statistics: AUC calculated with numpy.trapz (Python v3.9.10); significance testing via one-way ANOVA.
- All five compounds (acetaminophen, ibuprofen, TiO2, propranolol, metformin) negatively impacted E. coli MG1655 growth over 24 h, primarily reducing maximum OD, across a range of concentrations including environmentally relevant ones; effects were significant versus no-compound controls (p < 0.05, one-way ANOVA).
- Concentration-dependence was limited for most compounds; TiO2 showed a stronger effect at 100 µg/mL. Example AUC comparison concentrations included: 1 ng/mL acetaminophen, 5 ng/mL ibuprofen, 1 µg/mL TiO2, 0.5 ng/mL propranolol, 0.5 ng/mL metformin.
- Transcriptomics under 50 µg/mL ibuprofen identified 16 significantly upregulated genes. Notable hits: insA (IS2 element protein; logFC ~4.25), nikA (nickel ABC periplasmic binding; logFC ~2.54), stress/acid resistance genes yhcN (~1.40), yhiM (~1.34), bhsA (~1.16), nitrate reductase subunit nirB (~1.07), and multidrug efflux components mdtE (~1.29), emrA (~1.09), emrD (~1.07). The pattern suggests activation of stress responses and increased efflux activity during ibuprofen exposure.
- Co-exposure assays: Ibuprofen did not alter MICs of ethidium bromide, ampicillin, ciprofloxacin, chloramphenicol, trimethoprim, or colistin in MG1655 or ATCC 25922. FIC indices indicated no synergy or antagonism (e.g., MG1655 FICs: EtBr 2, AMP 3, CIP 2, CHL 2, TMP 3, CST 1.5).
- Long-term (30-day) exposure to each compound did not improve growth; instead, evolved populations generally exhibited decreased maximum OD in the presence of the selection compound relative to the ancestor, with significant differences for most populations (p < 0.05), most pronounced for ibuprofen and TiO2. Reduced growth persisted at 100× compound concentrations and after a 7-day recovery without compounds, arguing against transient toxicity effects.
- Whole-genome analyses of evolved populations revealed no parallel (shared) SNPs across independent lineages within treatments. Sporadic variants (e.g., recQ and ygeA) appeared in single replicates under acetaminophen exposure, consistent with drift. Variations in ldrA occurred in one replicate per condition (including a control); IS element inventories were unchanged and showed no evidence of transposition relative to the ancestor.
- MICs of the ibuprofen-evolved isolate were the same as or within one doubling dilution of the ancestor across all antibiotics tested (e.g., MG1655 ancestor MICs: EtBr 512 mg/L; AMP 4 mg/L; CIP 0.0156 mg/L; CHL 8 mg/L; TMP 0.25 mg/L; CST 4 mg/L; ibuprofen-evolved AMP 8 mg/L), indicating no selection for cross-resistance.
The study demonstrates that several non-antibiotic pharmaceuticals and TiO2 at environmentally relevant concentrations exert measurable toxicity against E. coli MG1655, evidenced by reduced growth yields. Despite acute stress responses—including upregulation of efflux systems (MdtEF-TolC, EmrAB-TolC), stress tolerance genes, and nitrate reduction components under ibuprofen—30-day selection did not result in convergent genetic adaptation, fixation of mutations, or altered antibiotic susceptibility. The findings indicate that, under the tested conditions, these compounds impose stress but not a selection pressure sufficient for adaptive genetic changes linked to cross-resistance. Efflux activation and stress response pathways may mitigate intracellular accumulation and reduce selective pressure. The lack of synergy with antibiotics during co-exposure and unchanged MICs after chronic ibuprofen exposure further suggest low risk of co-selection for antibiotic resistance in this model. Nonetheless, ecological implications remain: chronic exposure could alter community composition by disadvantaging sensitive taxa, and effects may vary across species and strains. These outcomes emphasize the need to evaluate broader bacterial diversity, fluctuating environmental concentrations, and complex effluent mixtures when assessing environmental AMR risks.
Non-antibiotic pharmaceuticals (acetaminophen, ibuprofen, propranolol, metformin) and TiO2 exhibit intrinsic toxicity toward E. coli MG1655, reducing growth at environmentally relevant concentrations. Ibuprofen induces stress responses and upregulates multidrug efflux genes, but prolonged exposure did not drive consistent genetic changes nor select for cross-resistance to a panel of antibiotics. Co-exposure of ibuprofen with antibiotics showed no synergy or antagonism and did not alter MICs. Overall, under laboratory conditions and timescales tested, these compounds are unlikely to select for antibiotic cross-resistance in E. coli. Future work should: (1) expand to diverse environmental and clinical strains and additional species; (2) test complex, variable effluent mixtures and concentration fluctuations; (3) extend selection timescales and ecological complexity (e.g., biofilms, communities); and (4) assess real-world environmental samples to validate laboratory findings.
The study used a single laboratory E. coli strain (K-12 MG1655), and responses may be strain- or species-specific. Only a small panel of non-antibiotic compounds was examined, with transcriptomics focused solely on ibuprofen. Environmental exposures were modeled at fixed concentrations and laboratory conditions that may not capture temporal fluctuations, community interactions, or biofilm contexts in natural settings. The 30-day selection period might be insufficient for detecting rare adaptive events, and only select antibiotics were tested for cross-resistance. Genomic analyses focused on SNPs and IS elements; other genomic changes (e.g., gene amplification, epigenetic regulation) were not comprehensively assessed.
Related Publications
Explore these studies to deepen your understanding of the subject.