Medicine and Health
NEK2 inhibition triggers anti-pancreatic cancer immunity by targeting PD-L1
X. Zhang, X. Huang, et al.
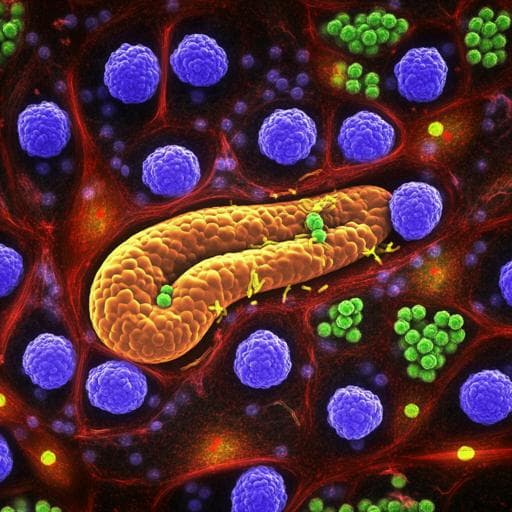
Pancreatic ductal adenocarcinoma (PDAC) is a lethal malignancy with increasing incidence and mortality despite therapeutic advances. Immune checkpoint blockade targeting PD-1/PD-L1 has shown success in several cancers, but PDAC responses have been limited, with trials reporting 0% objective response for durvalumab monotherapy and minimal benefit with combinations. Post-translational modifications (PTMs) such as glycosylation and phosphorylation critically regulate PD-L1 stability and function, influencing therapeutic efficacy. Prior studies show EGF signaling via B3GNT3 promotes PD-L1 N-glycosylation (N192/N200/N219) to stabilize PD-L1 by preventing GSK3β-mediated phosphorylation and BTRCP-dependent degradation; metformin-activated AMPK phosphorylation at S195 induces aberrant glycosylation and ER-associated degradation of PD-L1. NEK2, a serine/threonine kinase involved in cell cycle regulation, is overexpressed in multiple cancers including PDAC and linked to poor prognosis, but its role in cancer immune resistance is unknown. The study investigates whether NEK2 regulates PD-L1 and impacts anti-tumor immunity in PDAC, and whether NEK2 inhibition can sensitize PD-L1 blockade.
The paper reviews evidence that PD-L1 PTMs regulate its stability and immunosuppressive function: EGF upregulates B3GNT3 to enhance N-glycosylation at N192/N200/N219, stabilizing PD-L1 by blocking GSK3β phosphorylation (T180/S184) and subsequent BTRCP-mediated ubiquitination; EGFR inhibition enhances PD-L1 blockade efficacy. AMPK phosphorylation at S195 leads to abnormal glycosylation and ER-associated degradation of PD-L1, boosting antitumor immunity. Additional literature indicates kinases involved in cell cycle (CDK4/6, CDK5) modulate PD-L1 abundance or transcriptional control, and their inhibitors can synergize with PD-1/PD-L1 blockade. These findings motivate exploring NEK2 as a potential kinase regulator of PD-L1 in PDAC.
Design: Combination of bioinformatic analyses, in vitro mechanistic experiments, and in vivo mouse models to determine NEK2's role in PD-L1 regulation and antitumor immunity.
- Bioinformatics: Analysis of TCGA PAAD (and other public datasets: ICGC, GTEx, GEPIA2, TISIDB, Kaplan-Meier Plotter, cBioPortal) to compare NEK family expression in tumor vs normal, correlate NEK2 with overall survival (OS), immune effector cell signatures, CD8+ T-cell status, and tumor mutational burden (TMB). GO enrichment for pathways associated with NEK2 overexpression.
- Clinical specimens: Paired PDAC and matched normal tissues; PDAC tissue microarray (n=156) for NEK2 and PD-L1 IHC, correlation (Spearman) with prognosis and clinicopathological features (vascular invasion, grade).
- Cell lines: KPC murine PDAC cells and human PDAC lines (e.g., SW1990, CFPAC-1). Generation of stable NEK2 knockdown (KD) using double nickase plasmids; transient transfection of PD-L1 mutants (T193/209A, T193/209D in mouse; T194/210A, T194/210D in human) and NEK2 kinase-dead mutant (K37R). Transfection via Lipofectamine 3000/Ultracruz; selection with puromycin.
- NEK2 inhibitor: NCL00017509 (potent reversible NEK2 inhibitor). In vitro: 10 µM for 24 h; in vivo dosing: subcutaneous tumors, 100 µg/mouse intratumoral three times weekly for 2 weeks; orthotopic model, 200 µg/mouse intraperitoneal three times weekly for 2 weeks.
- In vivo models: Subcutaneous implantation of KPC WT vs NEK2 KD cells into immunocompetent C57BL/6 and immunodeficient nude mice; assessment of tumor incidence, growth, weight, and survival (orthotopic implantation for survival). Treatment studies with NEK2 inhibitor and/or anti-PD-L1 antibody (InVivoMAb, 200 µg/mouse i.p.) in subcutaneous and orthotopic KPC models; randomization at tumor size 50–100 mm³, treatment three times weekly for 2 weeks.
- Immune profiling: Flow cytometry of tumor-infiltrating lymphocytes (TILs) for CD45, CD3, CD8, and intracellular Granzyme B, Perforin, IFN-γ, TNF-α after leukocyte activation; assessment of immunosuppressive populations in patient samples (CD11b, CD11c, CD15, CD68, HLA-DR) and intracellular NEK2.
- T cell cytotoxicity assay: Co-culture of KPC cells with mouse CD8+ T cells (ratio 1:4) with NEK2 inhibitor and/or anti-PD-L1; quantification of surviving cancer cells by crystal violet staining (OD570).
- Protein analyses: Western blotting for NEK2, phospho-NEK2, PD-L1, ubiquitin, GSK3β, phospho-GSK3β, ER markers (IRE1α, HSP90B1), EGFR, tags (Flag, GFP), loading controls. Co-immunoprecipitation (endogenous PD-L1–NEK2 interaction), GST pull-down with recombinant GST-PD-L1 and NEK2-His; Duolink in situ proximity ligation assay for PD-L1–NEK2 interaction localization.
- ER localization: ER microsome preparation and limited trypsinization with/without Triton X-100 to probe luminal vs cytosolic accessibility of PD-L1–NEK2 complex.
- Kinase assays: In vitro kinase reaction using recombinant PD-L1 WT and active NEK2 with ATP, detection by custom phospho-specific antibodies (pT193/pT209 in mouse; pT194/pT210 in human) generated via peptide immunization and affinity purification.
- PD-L1 stability and ubiquitination: Cycloheximide chase (20 µg/mL) to determine PD-L1 half-life with/without NEK2 inhibitor or NEK2 KD; proteasome inhibitor MG132 rescue (50–100 µM). Ubiquitination assays by IP of PD-L1 followed by anti-ubiquitin immunoblot.
- Glycosylation: Assessment of PD-L1 glycosylation status upon NEK2 overexpression (LC-MS proteomics and immunoblotting).
- Statistics: Student’s t-test for two-group comparisons; one-way and repeated-measures ANOVA for multiple groups; Spearman’s correlation; Kaplan–Meier survival with log-rank or Gehan-Breslow-Wilcoxon tests. P<0.05 significant. Data reported as mean ± SD from ≥3 biological replicates.
- NEK2 expression and prognosis: NEK2 is the most upregulated NEK family member in TCGA-PAAD. NEK2 protein elevated in PDAC vs matched normal by IHC; higher NEK2 correlates with worse prognosis in tissue microarray (p<0.0001). In TCGA, high NEK2 associates with inferior OS (HR=1.6; 95% CI 1–2.56; log-rank p=0.05). NEK2 expression significantly associates with poor OS in CD8+ T cell-enriched ("hot") PDAC (HR=4.25; 95% CI 1.45–12.43; p=0.0046) but not in CD8+ decreased ("cold") tumors (HR=0.75; p=0.29). High NEK2 correlates with vascular invasion (p=0.043) and poor differentiation (p=0.045).
- Immune dependence: NEK2 KD reduces resistance to T cell-mediated cytotoxicity in vitro and suppresses tumor growth in immunocompetent C57BL/6 mice, but not in nude mice. NEK2 KD tumors show increased CD8+ T-cell infiltration and effector function (Granzyme B, Perforin), and prolonged survival in immunocompetent mice (p<0.0001), with no survival difference in nude mice (p=0.33).
- NEK2 inhibition in vivo: NEK2 inhibitor pretreatment lowers tumor incidence and delays onset in C57BL/6 but not nude mice. Therapeutic NEK2 inhibition suppresses tumor growth and reduces tumor weight in immunocompetent but not nude mice, without affecting body weight. Treated tumors exhibit decreased PD-L1 expression and increased CD8+ T-cell infiltration.
- NEK2–PD-L1 relationship: NEK2 and PD-L1 alterations co-occur and their expression positively correlates in TCGA, paired clinical tissues, tissue microarrays (Spearman R=0.43; p<0.0001), and GEMM PDAC tumors. Endogenous co-IP, GST pull-down, and Duolink assays show direct interaction. ER fraction trypsinization supports localization of the interaction within the ER lumen.
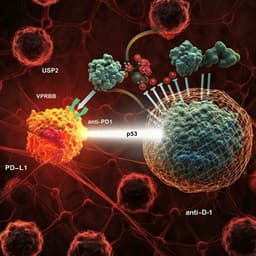
- Mechanism—stability via phosphorylation: NEK2 inhibition or KD reduces PD-L1 protein levels (total and membrane) and shortens PD-L1 half-life; NEK2 overexpression increases PD-L1 abundance. MG132 rescues PD-L1 levels under NEK2 inhibition/KD, indicating proteasome-mediated degradation. Ubiquitination of PD-L1 increases with NEK2 inhibition/KD. NEK2 influences PD-L1 more prominently than GSK3β in PDAC context.
- Phosphorylation sites: Two NEK consensus motifs (F/LXXS/T) identified near PD-L1 glycosylation sites; NEK2 directly phosphorylates PD-L1 at T194 and T210 (mouse T193/T209), demonstrated by in vitro kinase assays and phospho-specific antibodies, with phosphorylation reduced by NEK2 inhibition/KD. Non-phosphorylatable PD-L1 mutant (T193/209A) exhibits reduced PD-L1 levels, shortened half-life, and increased ubiquitination; phospho-mimetic (T193/209D) increases PD-L1 stability and reduces ubiquitination. NEK2 kinase-dead (K37R) loses regulatory effect.
- Combination therapy: NEK2 inhibitor plus anti-PD-L1 enhances T cell-mediated cytotoxicity in vitro versus monotherapies. In KPC-bearing mice, combination treatment significantly reduces tumor volume and weight compared to single agents, increases intratumoral CD8+ T-cell frequency and activation (Granzyme B, Perforin, IFN-γ, TNF-α), without affecting body weight. Similar results in orthotopic model; pharmacodynamic evidence confirms NEK2 inhibition in vivo.
The study addresses why PD-L1 blockade underperforms in PDAC by identifying NEK2 as a kinase that stabilizes PD-L1 through phosphorylation at T194/T210 within the ER, thereby sustaining immune evasion. Loss or inhibition of NEK2 reduces PD-L1 stability via enhanced ubiquitin-proteasome degradation, promotes CD8+ T-cell infiltration and function, and suppresses tumor growth in an immune-competent setting. The findings align with and extend prior work showing kinase-mediated control of PD-L1 PTMs, adding NEK2 to the network (alongside GSK3β, AMPK, JAK1). Clinically, NEK2 emerges as a prognostic biomarker particularly in immunologically "hot" PDAC and low TMB tumors, populations more likely to benefit from immunotherapy enhancement strategies. The synergy of NEK2 inhibition with PD-L1 blockade suggests a rational combination to overcome PDAC immunoresistance, analogous to benefits observed when combining CDK4/6 inhibitors with checkpoint antibodies in other cancers. Mechanistically, the proximity of T194 to S195 implies crosstalk with glycosylation steps that govern PD-L1 maturation and stability, offering additional intervention points.
NEK2 is overexpressed in PDAC and serves as a negative prognostic factor, especially in CD8+ T cell-enriched and low TMB tumors. NEK2 directly interacts with PD-L1 and phosphorylates T194/T210, stabilizing PD-L1 by preventing its ubiquitin-proteasome degradation in the ER. Genetic or pharmacologic NEK2 inhibition lowers PD-L1 levels, enhances antitumor T-cell immunity, and synergizes with PD-L1 blockade to reduce tumor burden in preclinical PDAC models. These results propose NEK2 as a therapeutic target and support combining NEK2 inhibitors with PD-L1 antibodies to improve immunotherapy efficacy in PDAC. Future work should include development/optimization of clinically viable NEK2 inhibitors or agents targeting PD-L1 T194/T210 phosphorylation, validation in additional PDAC models and immune subsets, biomarker-driven patient selection (immune "hot"/low TMB), and clinical trials to assess safety and efficacy.
The study is preclinical and relies on mouse models and cell lines; clinical efficacy and safety of NEK2 inhibitors in combination with PD-L1 blockade remain untested. Although a NEK2 inhibitor was used, off-target effects cannot be fully excluded, and pharmacokinetics/optimal dosing were not extensively profiled. The specific contribution of NEK2 in immune-suppressive myeloid populations (e.g., macrophages, DCs, MDSCs) was not functionally dissected. While phosphorylation at T194/T210 is implicated mechanistically, drug candidates specifically targeting these PD-L1 sites are not available and their specificity and safety are undetermined. The interplay between NEK2-mediated phosphorylation and PD-L1 glycosylation was suggested but not comprehensively mapped. Bioinformatic prognostic analyses, including TMB-stratified subsets, require prospective validation.
Related Publications
Explore these studies to deepen your understanding of the subject.