Medicine and Health
Monospecific and bispecific monoclonal SARS-CoV-2 neutralizing antibodies that maintain potency against B.1.617
L. Peng, Y. Hu, et al.
Discover the groundbreaking work by Lei Peng, Yingxia Hu, and their colleagues, as they unveil monoclonal antibodies that effectively neutralize SARS-CoV-2 variants. Their innovative approach, combining high-throughput single-cell sequencing and structural biology, offers new therapeutic alternatives against COVID-19 and its evolving strains.
~3 min • Beginner • English
Introduction
The study addresses the need for broadly effective therapeutic monoclonal antibodies against SARS-CoV-2, particularly as variants of concern (e.g., Alpha, Beta, Delta, Omicron) reduce vaccine and some antibody efficacy. The authors hypothesize that discovering potent RBD-targeting antibodies with distinct epitopes and multi-specific formats (bispecific) can enhance neutralization breadth and reduce viral escape. They aim to rapidly identify potent antibodies via immunization of mice with spike RBD followed by high-throughput single-cell BCR sequencing, characterize their binding and structures, and test efficacy against historical and variant SARS-CoV-2 in vitro and in vivo, including generating a humanized candidate for translational development.
Literature Review
The paper situates the work in the context of: (a) widespread use of vaccines and EUA monoclonal antibodies with emerging resistance among variants of concern; (b) noted transmission and immune evasion of B.1.1.7 (Alpha), B.1.351 (Beta), and B.1.617 (Kappa/Delta) lineages; (c) prior mAb discovery largely from convalescent human samples, versus immunization plus hybridoma approaches; and (d) recent adoption of high-throughput single-cell V(D)J sequencing to identify neutralizing antibodies against pathogens including SARS-CoV-2. Structural studies have shown many potent neutralizers block ACE2 by targeting RBD. The authors compare their antibodies to previously reported mAbs (e.g., 2H2, CV05-163, S2H13, CT-P59, BD23), noting distinct binding geometries relative to existing PDB structures.
Methodology
- Immunization and B cell isolation: C57BL/6J and BALB/c female mice (6–12 weeks) were immunized with SARS-CoV-2 RBD-His following a 28-day prime-boost protocol with CFA/IFA and a final i.p. boost. High-titer mice were selected by ELISA, and CD138+ plasma/progenitor B cells were isolated from spleen, lymph node, and bone marrow using magnetic microbeads.
- Single-cell BCR sequencing and analysis: 10x Genomics Single Cell V(D)J workflow was used to capture ~10,000 cells/sample. Libraries were sequenced (NovaSeq), processed with Cell Ranger, and clonotypes visualized in Loupe. Top enriched IgG1 heavy/light chain pairs were codon-optimized for human expression.
- Antibody engineering and expression: Variable regions were cloned into human IgG1 heavy and kappa light chain vectors (pFUSE). IgGs were expressed in Expi293F cells and purified by Protein A.
- Bispecific antibody generation: A bispecific antibody (Clone 16) combining variable regions from Clones 2 and 6 was produced using CrossMab “knobs-into-holes” (KiH) engineering to enforce correct heavy/light pairing and heterodimerization; expressed in Expi293F and purified.
- Humanization: Clone 2 was humanized (Clone 13A) via CDR grafting onto human frameworks with Vernier residue back-mutations guided by cryo-EM structures.
- Biophysical characterization: ELISA confirmed RBD binding. Binding kinetics were measured by BLI (Octet) and SPR (Biacore). Two SPR formats were used: NTA chip with RBD immobilized (avidity context) and CM5 chip with anti-human Fc capture of antibodies (monovalent affinity context).
- Structural biology: Fab fragments of Clones 2 and 6 were generated by papain digestion and purified. Cryo-EM grids of S ectodomain trimer with Fab were prepared and imaged on a Titan Krios/K3. Data were processed with RELION/cryoSPARC; models built with SWISS-MODEL, Chimera/ChimeraX, Coot, Refmac, PHENIX. Multiple S trimer conformational states per Fab were reconstructed at ~3 Å. Variant RBD homology models (Beta, Delta) were generated by SWISS-MODEL for epitope–mutation analysis.
- Functional assays: Cell–cell fusion inhibition assays used spike-expressing producer cells and hACE2 target cells. Pseudovirus neutralization employed HIV-1 or VSV-based SARS-CoV-2 S pseudotypes for WA1, B.1.351 (Beta), and B.1.617 (Delta lineage) with readouts by luciferase or GFP; IC50 values calculated from dose–response curves. Authentic virus neutralization used SARS-CoV-2 USA-WA1/2020 and Delta in BSL-3, with cytopathic effect/CellTiter-Glo or focus reduction assays.
- In vivo efficacy: K18-hACE2 transgenic mice were challenged intranasally with 2×10^3 PFU WA1 or Delta. Prophylactic dosing (20 mg/kg i.p.) occurred 24 h pre-challenge; therapeutic dosing at +18 h post-infection. Body weight and survival were monitored over 10 days, with statistics via two-way ANOVA and log-rank tests.
Key Findings
- Antibody discovery: Single-cell V(D)J sequencing of RBD-immunized mice identified enriched IgG clonotypes. From 11 top clones, two (Clones 2 and 6) showed strongest binding and neutralization.
- Binding kinetics:
• BLI (avidity context): Clone 2 KD ≈ 1.58 pM; Clone 6 KD ≈ 1.89 pM; dissociation phase not observed due to strong binding.
• SPR NTA (RBD immobilized; avidity): Clone 2 KD = 44.07 pM (kon 1.608×10^6 M^-1 s^-1, koff 7.089×10^-5 s^-1); Clone 6 KD = 148.4 pM (kon 3.773×10^6 M^-1 s^-1, koff 5.6×10^-4 s^-1).
• SPR CM5 (antibody capture; monovalent affinity): Clone 2 KD = 1.38 nM (kon 6.53×10^5 M^-1 s^-1, koff 8.97×10^-4 s^-1); Clone 6 KD = 2.27 nM (kon 6.11×10^5, koff 1.39×10^-3); Humanized Clone 13 KD = 10.6 nM (kon 1.8×10^6, koff 1.91×10^-2); Bispecific Clone 16 KD = 2.95 nM (kon 1.56×10^6, koff 4.6×10^-3).
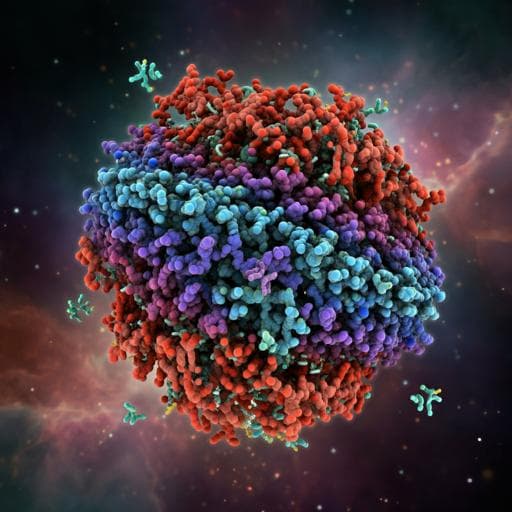
- Cryo-EM structures (~3 Å): Fabs 2 and 6 bind RBD at overlapping sites that block ACE2. Clone 2 complexes: S trimer with 2 RBDs up (60%) and 3 up (40%). Clone 6 complexes: 3 down (26%), 1 up (43%), 2 up (31%). Clone 6 additionally engages adjacent RBDs via CDRL1/FWR3 to stabilize down states and hinder ACE2, suggesting a second neutralization mechanism. Differences concentrated in CDRH3; Clone 6 has longer CDRH3 inserting into the RBD central groove. Both cover the ACE2 interface with distinct footprints.
- Pseudovirus neutralization: Clones 2, 6, and bispecific 16 potently inhibited WA1 with low ng/mL IC50. Against B.1.351 (Beta), potency was reduced (mid ng/mL IC50 for Clones 2/6; high ng/mL for Clone 16). Against B.1.617 lineage pseudovirus, all maintained strong potency with sub- to low-single-digit ng/mL IC50. A 2+6 cocktail was not superior to single clones but confirmed strong activity (single-digit ng/mL IC50 for WA1 and B.1.617, slightly reduced vs B.1.351).
- Authentic virus neutralization (in vitro): IC50 (WA1) — Clone 2: 108.3 ng/mL; Clone 6: 35.73 ng/mL; Clone 16: 131.8 ng/mL.
- In vivo efficacy (K18-hACE2):
• Prophylaxis (20 mg/kg, −24 h): Placebo (DPBS) mice developed severe disease; 7/8 died. All treated with Clone 2 (8/8) or Clone 6 (7/7) maintained weight and survived.
• Therapy (+18 h): Placebo (isotype hIgG1) developed severe disease; 4/5 lost weight. All treated with Clone 2 (5/5) or Clone 6 (5/5) maintained weight and survived.
- Humanized Clone 13A: Retained RBD binding (low double-digit nM by BLI) and potent pseudovirus neutralization (single-digit ng/mL IC50) against WA1 and B.1.617. Authentic virus assays showed potent neutralization of WA1 and Delta. Fold-drop in potency against Delta: REGN-10933 1.6×, Clone 13A 2×, Clone 2 4×, Clone 6 18×, REGN-10987 52×. In vivo, 13A protected 9/9 (WA1) and 8/8 (Delta) mice from lethal challenge; all placebo mice succumbed.
- Structural mutation analysis: Beta mutations K417N and E484K intersect with Fab interfaces (E484 central to CDRH1/H3; K417 contacts CDRL1 of Clone 6), explaining reduced potency vs B.1.351. Delta mutations L452R and T478K lie near but mainly outside the footprint; E484Q less disruptive than E484K, consistent with maintained potency against Delta. REGN-10987 epitope near left-shoulder loop affected by L452R explains its reduced Delta potency compared to Clone 2.
Discussion
The study demonstrates that RBD-targeting mAbs discovered via immunization coupled with single-cell V(D)J sequencing can achieve high affinity/avidity and broad neutralization, including against B.1.617 (Delta lineage). Cryo-EM analyses reveal both antibodies block ACE2 engagement, but with distinct geometries and a unique quaternary interaction of Clone 6 that stabilizes RBD-down states and interferes with adjacent up-RBDs, suggesting complementary mechanisms that can limit viral escape. Structural mapping rationalizes differential impacts of variant mutations: Beta mutations (K417N/E484K) disrupt Fab contacts and reduce potency, whereas Delta’s E484Q/L452R/T478K are less disruptive to these clones, correlating with maintained neutralization. The bispecific antibody retained high affinity but did not surpass parental clones, while humanization (Clone 13A) preserved potency and conferred robust in vitro and in vivo efficacy against WA1 and Delta. Collectively, epitope diversity, structural insights, and in vivo protection support these candidates as promising therapeutics resilient to key variant mutations.
Conclusion
This work reports rapid discovery of two potent SARS-CoV-2 neutralizing mAbs (Clones 2 and 6), a bispecific derivative (Clone 16), and a humanized candidate (Clone 13A). They exhibit picomolar to low-nanomolar binding, block ACE2, reveal distinct structural mechanisms of neutralization, and maintain strong activity against WA1 and B.1.617, with reduced but measurable activity against B.1.351. In vivo, both parental and humanized antibodies protect K18-hACE2 mice prophylactically and therapeutically. These antibodies expand the therapeutic repertoire against SARS-CoV-2 variants. Future work should evaluate safety/efficacy in humans, explore optimized combinations to further minimize escape, and assess breadth against newer variants.
Limitations
- Reduced neutralization potency against the B.1.351 (Beta) variant due to epitope-overlapping mutations (K417N, E484K), as indicated by structural analyses and pseudovirus data.
- The bispecific antibody (Clone 16) did not outperform parental monospecific clones, likely due to overlapping epitopes.
- Preclinical scope: efficacy was demonstrated in vitro and in K18-hACE2 mouse models; no clinical data are presented.
- Experiments were not blinded; some experiments had modest sample sizes; certain assays (e.g., SDS-PAGE display) were conducted once.
- Structural mutation impacts on emerging variants were inferred from homology models and require empirical confirmation across broader variant panels.
Related Publications
Explore these studies to deepen your understanding of the subject.