Medicine and Health
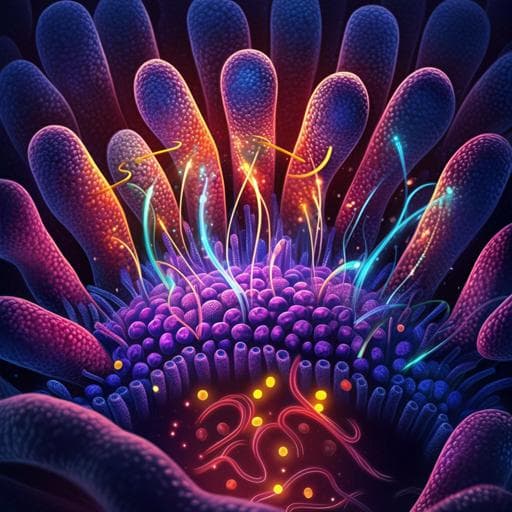
L-valine is a powerful stimulator of GLP-1 secretion in rodents and stimulates secretion through ATP-sensitive potassium channels and voltage-gated calcium channels
I. M. Modvig, M. M. Smits, et al.
This exciting study explores how L-valine boosts glucagon-like peptide 1 (GLP-1) release, revealing mechanisms that could influence metabolic health. Conducted by a team from the University of Copenhagen, the findings highlight the potential of L-valine in stimulating GLP-1, offering insights into gut responses.
Related Publications
Explore these studies to deepen your understanding of the subject.