Medicine and Health
Impact of Point-of-Care Rapid Diagnostic Tests on Antibiotic Prescription Among Patients Aged <18 Years in Primary Healthcare Settings in 2 Peri-Urban Districts in Ghana: Randomized Controlled Trial Results
A. Adjei, V. Kukula, et al.
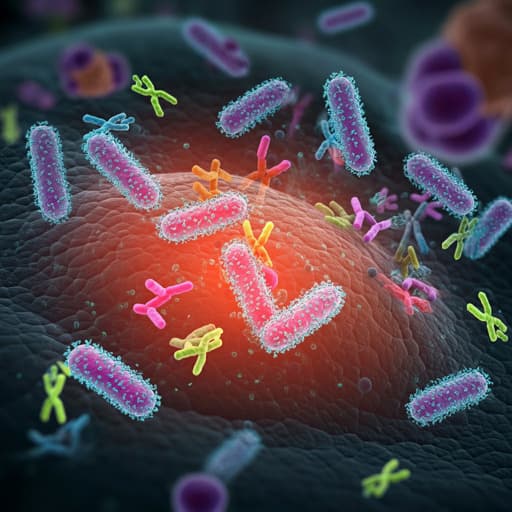
This study by Alexander Adjei and colleagues explores the impact of rapid diagnostic tests (RDTs) on antibiotic prescriptions for acute febrile illness in Ghanaian children. The intervention group showed an impressive 11% reduction in antibiotic use, particularly benefiting young children and those with respiratory symptoms. This research highlights the promise of employing point-of-care diagnostics and communication training to enhance clinical outcomes while combating inappropriate antibiotic prescriptions.
Related Publications
Explore these studies to deepen your understanding of the subject.







