Medicine and Health
Imaging and AI based chromatin biomarkers for diagnosis and therapy evaluation from liquid biopsies
K. Challa, D. Paysan, et al.
This groundbreaking study explores chromatin organization in PBMCs as game-changing biomarkers for cancer diagnosis and treatment evaluation. Authored by Kiran Challa, Daniel Paysan, Dominic Leiser, Nadia Sauder, Damien C. Weber, and G. V. Shivashankar, the research showcases a highly accurate machine learning pipeline capable of distinguishing healthy individuals from tumor patients and evaluating treatment effects. Discover the future of cancer diagnostics!
~3 min • Beginner • English
Introduction
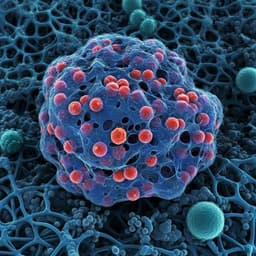
Tumors secrete diverse soluble factors into the tumor microenvironment, many of which enter the bloodstream. These circulating secretome signals vary with tumor type and stage and are modulated by therapies such as radiation. PBMCs sense and respond to these signals, undergoing epigenetic and chromatin remodeling linked to functional states. The study posits that 3D chromatin organization of PBMCs, captured via simple immunofluorescence imaging and analyzed with machine learning, can serve as patient-specific biomarkers for cancer diagnosis (healthy vs tumor and among tumor types) and for evaluating the efficacy of proton therapy over time. The purpose is to develop and validate an imaging and AI-based pipeline to quantify PBMC chromatin features as non-invasive biomarkers from liquid biopsies, addressing the need for resource-efficient tools beyond costly sequencing/proteomics and enabling timely, treatment-responsive assessment.
Literature Review
Prior liquid biopsy biomarkers include cytokines, growth factors, exosomes, circulating tumor DNA, and circulating tumor cells, as well as transcriptomic and proteomic signatures from blood cells. However, these approaches can be resource-intensive and often suited to later stages. Epigenetic chromatin remodeling governs immune cell gene regulation, and specific PBMC chromatin conformations have been proposed as cancer diagnostics. PBMC activation involves chromatin remodeling and DNA methylation changes, with tumor-secretome-driven dysfunctional states in T cells reflected in chromatin accessibility differences. Integrative single-cell RNA-seq and genetic studies link immune cell epigenetics to disease development. Imaging-based assessment of nuclear architecture and chromatin, coupled with machine learning, has detected subtle signal-induced chromatin alterations in prior studies, motivating a streamlined imaging approach for PBMC-based cancer biomarkers and therapy monitoring.
Methodology
Study design: Blood was collected from 10 healthy donors and 40 tumor patients (10 pan-tumor for healthy vs tumor classification; 30 patients—10 each with meningioma, glioma, head and neck cancers—undergoing proton therapy). For the therapy cohort, samples were obtained at three time points: prior to, during, and at the end of therapy (~6 weeks). Ethics approval (EKNZ 2021-00481) and informed consent were obtained.
PBMC isolation: Density-gradient centrifugation (Lymphoprep in SepMate-50). PBMCs washed, fixed (4% PFA), and prepared for imaging; surplus stored in liquid nitrogen.
Immunostaining and microscopy: Cells adhered on poly-L-lysine–coated coverslips, permeabilized, blocked, and stained for DAPI (DNA), γH2AX (DNA damage), Lamin A/C (nuclear architecture), and surface markers CD3, CD4, CD8 (plus CD16 in antibody list). Imaging by Leica Stellaris confocal, 63×/1.4 NA oil; voxel resolution 0.09 µm (xy), 0.5 µm (z).
Image processing: Multichannel images converted to TIFF; DAPI intensities range-normalized. Nuclei segmentation performed via 2D preprocessing (median filter, gamma adjustment, Otsu thresholding, size and border filters), guiding 3D crops; background removed using dilated convex hull masks. 3D nuclear masks obtained using the Chan–Vese active contour algorithm with post-filters on object size and height.
Cell segmentation: Approximate cell masks derived by dilating nuclear masks (12 px xy, 2 px z) to capture pericellular signal.
Feature extraction: Using 2D/3D nuclear masks on DAPI to quantify nuclear morphology and chromatin organization (chrometric features: e.g., nuclear volume, heterochromatin/euchromatin metrics, curvature, concavity, texture, moments). Protein marker intensities quantified by descriptive statistics within masks. Full feature list in public GitHub repository. γH2AX foci detected in 2D max-projections using intensity thresholding (≥2.5 SD above mean), size filter, watershed, and artifact removal.
Cell type identification: Marker positivity (CD3, CD4, CD8) determined by intensity sums within nuclear-proximal masks on 2D projections, normalized by projected cell area; thresholds per sample identified via two-component Gaussian mixture models to assign positive/negative labels.
Data preprocessing and sampling: Highly correlated features (|Pearson r|>0.8) removed. Balanced subsampling enforced equal numbers across conditions and equal representation per patient to avoid patient dominance. Sampling examples: 216 PBMCs per donor for healthy vs tumor (n=2160 per group); 240 PBMCs per patient for tumor-group comparisons and for each treatment time point; similar sampling for CD3+ vs CD3− analyses.
Batch effect control: tSNE visualizations assessed; no clustering by patient sample observed.
Classification and statistics: Random forest classifiers (RFCs) trained on chrometric features; performance evaluated as balanced accuracy using stratified leave-one-patient-out cross-validation. Random baselines via label permutation. Feature importance assessed via Gini importance; group differences via Welch’s t-tests with Benjamini–Hochberg correction. Ablation studies evaluated impact of number of patients and number of PBMCs per patient on performance.
Key Findings
- Healthy vs tumor discrimination: Single-cell RFC achieved average accuracy 0.77 (±0.10), specificity 0.77 (±0.09), sensitivity 0.78 (±0.11). With aggregation to patient-level majority vote, achieved 100% correct patient classification. Even training on PBMCs from as few as one control and one tumor patient yielded 0.72 (±0.03) accuracy on held-out patients. Key discriminative features included nuclear volume, shape/concavity, heterochromatin content; tumor PBMCs showed reduced Lamin A/C levels and increased γH2AX foci relative to controls.
- Tumor group identification: Among meningioma, glioma, and head & neck tumors, single-cell RFC average accuracy was 0.78 (±0.25). Class-wise accuracies: head & neck 0.89, meningioma 0.75, glioma 0.69. Frequent confusion between meningioma and glioma suggested similar PBMC chromatin states for brain tumors. Patient-level majority vote accuracy was 93% (28/30 patients correctly classified). Distinctive features across groups included nuclear volume, heterochromatin content (HC/EC ratio), concavity, and nuclear boundary curvature; head & neck patients exhibited significantly increased nuclear/heterochromatin volumes and more γH2AX foci.
- Therapy time point classification: Within each tumor group, RFC distinguished PBMCs from prior, during, and end of proton therapy with balanced accuracies: meningioma 0.82 (±0.09), glioma 0.83 (±0.12), head & neck 0.64 (±0.10). Glioma PBMCs showed clear separability across all time points (suggesting immediate reflection of therapy), whereas meningioma and head & neck showed partial confusion between prior and during (suggesting delayed reflection).
- Therapy-associated chromatin changes: Nuclear volume, heterochromatin content, and nuclear curvature variability decreased over the course of therapy across all tumor groups, trending toward healthy levels. Lamin A/C expression increased and γH2AX foci decreased over therapy, consistent with recovery and reduced DNA damage.
- Loss of tumor-type signature during therapy: An RFC trained per time point to classify tumor group achieved 77% accuracy pre-therapy but performed no better than chance during or at end of therapy, indicating diminishing tumor-specific chromatin signatures in PBMCs as therapy progressed.
- PBMC subset dynamics and cell-type specificity: Prior to therapy, CD4+CD8− cells were decreased and CD4−CD8+ cytotoxic cells increased in tumor patients vs controls; CD8+ abundance further increased during therapy. CD4+CD8+ cells were more abundant in tumor patients and increased during therapy. An RFC distinguished CD3+ vs CD3− PBMCs with 0.77 (±0.04) accuracy, showing intrinsic chromatin differences between subsets. However, therapy-related chromatin, Lamin A/C, and γH2AX changes were similar in CD3+ and CD3− subsets, indicating results were not solely due to shifts in cell-type composition.
Discussion
The findings demonstrate that PBMC chromatin organization acts as a sensitive integrator of circulating tumor secretome signals and therapy-induced changes. Imaging-based chromatin features coupled with machine learning provide a resource-efficient, scalable alternative to sequencing/proteomic biomarkers, enabling accurate discrimination between healthy and tumor states, differentiation among certain tumor types, and real-time monitoring of proton therapy effects. The robust single-cell performance and perfect patient-level aggregation for healthy vs tumor, along with high patient-level accuracy for tumor type classification, underscore clinical potential. Therapy-induced convergence of PBMC chromatin towards healthy profiles, increased Lamin A/C, and reduced DNA damage collectively reflect systemic response to effective treatment. While head & neck tumors showed somewhat lower separability across time points, glioma PBMCs responded promptly, suggesting tumor-specific kinetics of systemic signal normalization. The similarity between glioma and meningioma PBMC chromatin states aligns with known brain tumor secretome commonalities. Importantly, cell-type–specific analyses indicate that chromatin alterations are consistent across major PBMC subsets and not explained solely by changes in subset abundance. Together, these results support using PBMC chromatin as a non-invasive biomarker for diagnosis and therapy evaluation.
Conclusion
This work introduces an imaging and AI-based pipeline for deriving chromatin biomarkers from PBMCs in liquid biopsies. The approach accurately distinguishes healthy from tumor patients, separates tumor groups at high accuracy, and sensitively tracks proton therapy effects over time. Key biomarkers include nuclear volume, heterochromatin content, nuclear boundary concavity/curvature, Lamin A/C levels, and γH2AX foci. The method offers a streamlined, cost-effective complement to molecular assays. Future directions include larger, multi-center clinical trials to validate diagnostic and longitudinal performance, exploration of finer PBMC subset resolution (e.g., via sorting and expanded marker panels) to potentially enhance tumor-type discrimination, and broader evaluation across therapies and cancer types to generalize biomarker utility.
Limitations
- Cohort size and composition are limited (10 healthy; 40 tumor patients, with 30 in therapy cohort), warranting larger clinical trials for generalizability and to assess tumor-specific response kinetics.
- Imaging-derived features are sensitive to PBMC storage, sample preparation, and microscopy settings, necessitating stringent standardization for reproducibility and cross-site deployment.
- Tumor group separability varied (e.g., lower for glioma vs meningioma; head & neck time-point classification lower), indicating potential overlap in PBMC chromatin responses and need for additional features or modalities.
- Cell-type labeling was based on imaging intensity thresholds and limited markers; more granular immune subset characterization may refine diagnostic power.
- Analyses enforced balanced subsampling; real-world class imbalance and heterogeneous sampling may affect performance.
- Study focused on patients undergoing proton therapy; applicability to other treatments and earlier disease stages requires further validation.
Related Publications
Explore these studies to deepen your understanding of the subject.