Medicine and Health
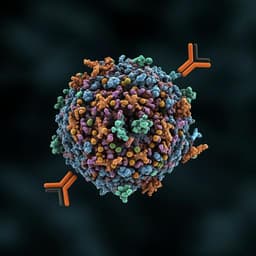
Human antibodies targeting a *Mycobacterium* transporter protein mediate protection against tuberculosis
A. Watson, H. Li, et al.
This exciting study explores how antibodies can protect against *Mycobacterium tuberculosis* during active tuberculosis. Researchers, including Avia Watson and Hao Li, developed monoclonal antibodies that significantly reduced bacterial levels in infected models. Their findings shed light on the potential for immunotherapy in tuberculosis treatment.
~3 min • Beginner • English
Introduction
Exposure to Mycobacterium tuberculosis results in a spectrum of outcomes, including active tuberculosis (ATB) disease. While both innate and adaptive immunity contribute to control of Mtb, the role of humoral immunity, particularly antibodies, remains debated. Previous studies suggest antibodies may be protective in some exposed individuals and that certain vaccine-induced antibody responses correlate with protection. During active disease, higher anti-lipoarabinomannan titers have correlated with reduced severity, and B cell dysfunction appears reversible after treatment. Serum antibodies against the Mtb phosphate transporter PstS1 are detectable during active infection, but antibodies isolated from ATB patients had not been functionally characterized and their antibacterial effects were unclear. To address this gap, the study investigates B cell responses during ATB focused on PstS1, isolating monoclonal antibodies (mAbs) to define specificity, function, and structural epitopes and to test antibacterial activity ex vivo and in vivo.
Literature Review
Prior work implicates antibodies in protective immunity against Mtb in subsets of individuals and in vaccine contexts, though findings have been inconsistent and the contribution of humoral responses remains controversial. Elevated antibody titers to glycolipid antigens like LAM have associated with decreased disease severity in ATB. Evidence indicates B cell dysfunction during ATB that normalizes post-therapy, and sera from ATB patients contain antibodies recognizing PstS1. However, functional activities of such antibodies against Mtb were not previously defined, and structural characterization of human anti-Mtb mAbs has been limited. Earlier molecular profiling of human B cell responses suggested isotype-dependent effects, with IgA linked to inhibition in vitro, but lacked in vivo validation and detailed antigen-binding mechanisms.
Methodology
- Human subjects and serology: Recruited 12 in-patients with ATB and screened sera by ELISA against Mtb lysates and selected surface-exposed proteins (including PstS1) to identify strong responders. Donor P.4, with the strongest anti-PstS1 response, was selected for monoclonal antibody isolation. Additional cohort data included 26 ATB patients versus 20 controls for broader serology.
- B cell isolation and mAb generation: Isolated PBMCs from donor P.4. Single-cell sorted CD19+ IgG+ PstS1+ memory B cells (~0.5% of IgG+ B cells). Amplified 102 heavy and 90 light chains by single-cell PCR, recovering 85 native heavy–light chain pairs. Sequence analysis identified five clonal families among 16 sequences. Expressed nine IgG1 mAbs from four clones; assessed binding to recombinant PstS1 and Mtb lysates by ELISA and to whole bacteria.
- Germline reversion and chain-swap chimeras: Inferred unmutated common ancestor (germline) versions of p4-36 and p4-163 and generated heavy-/light-chain swapped chimeras to assess contributions of somatic hypermutation in each chain to antigen binding by ELISA.
- Ex vivo functional assays: Evaluated mAb effects in THP-1 macrophage infection with H37Ra for bacterial entry and intracellular binding. Assessed antibacterial activity in a whole blood mycobacterial growth inhibition assay (MGIA) using BCG and pathogenic Mtb, measuring CFU after 96 h. Tested dose responses and compared active mAbs (p4-36, p4-163) to other anti-PstS1 mAbs (e.g., p4-31, p4-141). Probed mechanism via Fc dependence using IgG1-N297A aglycosylated variants and FcγR blocking (CD16/FcγRIII and CD32a/b, FcγRIIA/IIB). Assessed contributions of T cells by depleting CD3+, CD4+, CD8+ subsets and blocking MHC class II.
- Structural biology: Generated Fab fragments for p4-36 and p4-163 (structural analysis ultimately performed with clonal variant p4-170). Determined crystal structures of PstS1 in complex with Fab p4-36 at 2.1 Å (PDB ID 7DNM) and PstS1 with Fab p4-170 at 2.4 Å (PDB ID 7DMZ). Mapped epitopes, characterized interaction interfaces (hydrogen bonds, salt bridges, van der Waals contacts), and validated key contact residues by PstS1 point mutations and binding assays.
- Structural modeling: Modeled PstS1 binding to the PstA–B–C transporter complex by superimposition on a related ABC transporter (MetNIQ, PDB 6CVL) to assess whether antibody binding occludes complex assembly or function.
- In vivo efficacy: Prophylactically administered mAbs (0.5 or 1 mg per mouse, i.p.) to Balb/c mice 5 h prior to aerosol infection with Mtb. After 2 weeks, quantified lung bacterial burden (CFU). Compared p4-36 and p4-163 (alone or together) to isotype control across independent experiments.
- Additional experimental details: ELISA coating and detection conditions, flow cytometry staining of bacteria/cells, and MGIA processing parameters are described to ensure reproducibility. Data deposition includes PDB accessions for structures and GenBank accessions for antibody sequences.
Key Findings
- Identification of anti-PstS1 mAbs: From donor P.4, 85 paired mAbs were recovered; nine were expressed from four clonal families. Most mAbs bound recombinant PstS1 and Mtb lysates with nanomolar affinity by ELISA; p4-36 and p4-163 showed strongest lysate and whole-bacterium binding.
- Somatic hypermutation is required for binding: Germline-reverted variants p4-36(g) and p4-163(g) showed markedly reduced binding to PstS1 and Mtb lysates compared to mature mAbs. Chain-swap analysis indicated p4-36 binding depended more on light-chain mutations, whereas p4-163 depended more on heavy-chain mutations.
- Ex vivo inhibition of mycobacterial growth: In human whole-blood MGIA, p4-36 and p4-163 significantly restricted growth of BCG and pathogenic Mtb after 96 h, whereas other anti-PstS1 mAbs did not, indicating activity is not predicted solely by ELISA binding. Activity was not strictly dose-dependent in tested ranges.
- FcγR-dependent mechanism: The aglycosylated IgG1-N297A variants of p4-36 and p4-163 lost inhibitory activity in MGIA. Blocking FcγRIII (CD16) and FcγRIIA/IIB (CD32a/b) diminished mAb-mediated CFU reduction, while T cell depletion or MHC II blockade had no effect, implicating FcγR-mediated effector functions (e.g., opsonization) rather than T cell–dependent mechanisms.
- Structural epitopes on PstS1: The p4-36 epitope is a contiguous alpha-helical region (residues 136–145, with contacts involving 136–137 and 139–140) with a contact area of ~583 Ų, dominated by van der Waals and hydrogen bonds primarily from CDRL1, CDRL3, and CDRH3; includes a salt bridge between Asp36 of CDRL1 and Lys139 of PstS1. The clonal variant p4-170 (97.6% identity to p4-163) binds a highly discontinuous epitope (~977 Ų) proximal to the phosphate-binding site between PstS1 domains I and II, engaging multiple residues across three helices and four loops via hydrogen bonds and four salt bridges (e.g., Glu85–Arg55, Glu88–Arg55, Lys268–Asp77, Asp279–Arg54).
- Epitope validation and functional implications: PstS1 point mutations S246G, K268A, and D279A reduced binding of p4-170/p4-163-like mAbs but not p4-36; mutations K136A, D139A, D140A in the alpha-helix reduced p4-36 binding. Structural modeling indicated neither p4-36 nor p4-170 binding would block assembly of the PstA–B–C–S transporter complex.
- In vivo efficacy: Prophylactic administration of p4-36 and p4-163 to Balb/c mice prior to aerosol Mtb infection reduced lung bacterial burden compared to control. Reported effects included approximately 1.5 log CFU reduction after 2 weeks in treated groups, consistent with ex vivo MGIA findings. The abstract also describes about a 50% reduction in bacterial lung burden.
- Overall: Naturally elicited human anti-PstS1 IgG mAbs can mediate FcγR-dependent inhibition of Mtb ex vivo and reduce bacterial burden in vivo, with distinct, non-competing epitopes suggesting potential for combinatorial therapy.
Discussion
The findings demonstrate that during active tuberculosis, humans can generate somatically mutated IgG antibodies against the Mtb phosphate transporter subunit PstS1 with functional antibacterial activity. The ex vivo and in vivo data indicate that protection is mediated via Fcγ receptor–dependent effector mechanisms rather than direct inhibition of transporter function, as structural modeling showed no interference with Pst complex assembly. Distinct epitopes targeted by p4-36 (a compact alpha-helical site) and p4-163/p4-170 (a large discontinuous site near the phosphate-binding pocket) suggest complementary, non-competing binding that could be leveraged in combination therapies. The relatively modest somatic hypermutation in these mAbs, together with their functional activity, supports the notion that protective humoral responses may arise during ATB but could develop late relative to infection dynamics. These results contribute to resolving the debate over the role of antibodies in TB by providing molecular, functional, and structural evidence that human anti-PstS1 antibodies can inhibit Mtb growth and reduce bacterial burden, highlighting PstS1 as a promising target for antibody-based interventions and vaccine design.
Conclusion
This study isolates and characterizes human monoclonal antibodies against the Mtb antigen PstS1 from a patient with active TB, identifies two antibodies (p4-36 and p4-163) with significant ex vivo inhibitory activity and in vivo efficacy in mice, and defines their distinct structural epitopes on PstS1. The antibacterial effects are FcγR-dependent and do not result from blocking Pst transporter assembly. These results position PstS1 as a viable target for therapeutic antibodies and vaccines and suggest that combinations of non-competing anti-PstS1 mAbs may offer synergistic benefits. Future work should delineate precise effector mechanisms (killing versus growth restriction), evaluate therapeutic (post-infection) dosing and different delivery regimens, optimize Fc engineering for enhanced effector function, assess breadth against diverse Mtb strains, and validate efficacy in additional, more pathophysiologically relevant animal models.
Limitations
- Source mAbs were derived from a single donor with active TB, limiting generalizability.
- Mouse efficacy studies used prophylactic administration prior to infection and the Balb/c model, which does not recapitulate human lung granulomas; therapeutic efficacy post-infection remains to be shown.
- Ex vivo MGIA, while physiologically relevant, may not fully model in vivo complexity; activity was not strictly dose-dependent in tested ranges.
- Structural analysis for clone 1 used p4-170 (a close variant of p4-163) due to crystallization constraints, which may not capture all features of p4-163.
- Mechanistic studies indicate FcγR dependence but do not distinguish between enhanced uptake with intracellular killing versus restriction of replication.
- Several methodological descriptions show OCR or typographical inconsistencies; some affiliation assignments and minor experimental parameters may be ambiguous from the provided text.
Related Publications
Explore these studies to deepen your understanding of the subject.