Medicine and Health
Hamster model for post-COVID-19 alveolar regeneration offers an opportunity to understand post-acute sequelae of SARS-CoV-2
L. Heydemann, M. Ciurkiewicz, et al.
SARS-CoV-2 has caused hundreds of millions of infections with substantial mortality. A significant fraction of survivors develop post-acute sequelae of SARS-CoV-2 (PASC), with persistent respiratory symptoms such as shortness of breath and dyspnea months after infection. While lung fibrosis occurs in a subset of patients after severe COVID-19, it does not fully explain all respiratory PASC symptoms. An additional mechanism is impaired gas exchange due to incomplete or protracted alveolar regeneration following diffuse alveolar damage (DAD), in which AT1 and AT2 cells are injured and replaced through regenerative processes. Recent work in lung injury models shows that regeneration involves an intermediate cell state—the alveolar differentiation intermediate (ADI)—and recruitment of airway progenitors after severe injury. ADI cells, characterized by CK8 expression and activation of NFκB/TP53 and EMT-related programs, can transiently appear during normal repair but abnormally accumulate in fibrosis and severe COVID-19. However, the dynamics, fate, and persistence of ADI cells after SARS-CoV-2 infection remain unclear due to limited longitudinal human sampling. This study addresses these gaps by using SARS-CoV-2-infected Syrian golden hamsters to define morphological, phenotypical, and transcriptomic features of alveolar regeneration, test the involvement of airway-derived progenitors, and assess whether persistent ADI cells and fibrosis arise post-infection, thereby informing mechanisms relevant to PASC.
Prior studies demonstrate that after lung injury, AT2 cells typically regenerate AT1 cells, but severe injury recruits airway progenitors (including basal and club cell populations) to repair alveoli. A transitional ADI state (KRT8/CK8-high) occurs during AT2-to-AT1 differentiation and is transient in normal repair but accumulates in idiopathic pulmonary fibrosis and has been reported in severe COVID-19 lungs. ADI cells exhibit features of senescence, NFκB/TP53 activation, EMT-related gene programs, and pathway involvement of TGF-β, Notch, and Wnt/β-catenin. COVID-19 autopsies revealed abundant ADI cells and basal cell ‘pods,’ suggesting dysregulated regeneration. Animal models such as hamsters phenocopy moderate to severe COVID-19 and allow sequential analyses, yet detailed characterization of alveolar regeneration and ADI dynamics in hamsters had been lacking.
Animal model: Eight- to ten-week-old male and female Syrian golden hamsters (n=80 total; groups of 10 per time point per condition) were acclimatized under BSL-3 conditions and intranasally infected with 10^4 pfu of ancestral SARS-CoV-2 (SARS-CoV-2/Germany/Hamburg/01/2020) or mock (PBS). Time points: 1, 3, 6, and 14 days post infection (dpi). Animals (n=10/group/time) were euthanized; right lung lobes were collected for histology and TEM. Sexes were pooled without sex-based analysis. Histopathology and immunohistochemistry (IHC): Formalin-fixed paraffin-embedded sections were stained with HE and Azan trichrome. IHC detected SARS-CoV-2 nucleoprotein (NP), Iba-1 (macrophages/histiocytes), AT2 cells (pro-surfactant protein C, proSP-C), ADI cells (cytokeratin 8, CK8), airway basal cells (cytokeratin 14, CK14), club cells (SCGB1A1), and M2 macrophages (CD204). Double-label immunofluorescence assessed transitional states and lineage relationships: proSP-C/CK8 (AT2↔ADI), CK8/TP53 (cell cycle arrest), CK14/proSP-C (airway→AT2), CK14/CK8 (airway→ADI), CK14/SCGB1A1 (airway→club). Negative controls used isotype/serum substitutions. Antibody panels detailed in Supplementary Tables. Transmission electron microscopy (TEM): Glutaraldehyde-fixed tissue underwent osmium postfixation, dehydration, resin embedding, ultrathin sectioning, and uranyl/lead staining. Morphology was assessed to identify cells with combined AT1/AT2 ultrastructural features supporting ADI→AT1 transition. Digital image analysis: Whole-slide images (Olympus VS200) analyzed in QuPath. ROIs defined for airways, blood vessels, affected and non-affected alveoli, and artifacts. Automated detection quantified positive cells and areas. Epithelial proliferation and subpleural fibrosis quantified as percent of total lung area. Human samples: Lung tissues from three lethal COVID-19 ARDS patients and one non-COVID bronchopneumonia (lobectomy) were examined for ADI markers (CK8, proSP-C) and TP53. Single-cell RNA-seq reanalysis: Public dataset GSE162208 (hamster lungs at 5 and 14 dpi). Seurat (v3.2.0) preprocessing: filtering (nFeature_RNA>200,<2500; percent.mt<5), normalization, variable feature selection (2000), scaling, PCA, neighbor graph, clustering (resolution 0.5) and UMAP. Alveolar clusters identified using Rtkn2 (AT1) and Lamp3 (AT2), then re-clustered (7 clusters at 5 dpi; 11 at 14 dpi). Candidate marker lists (AT1, AT2, ADI, club, ciliated) curated from DEGs and literature, refined by specificity (feature/ridge plots). Module scores (AddModuleScore) computed for cell-type markers and GSEA Hallmark pathways (p53, DNA repair, TGF-β, Notch, Wnt/β-catenin, EMT, angiogenesis, G2M). Statistical analyses used Mann-Whitney U tests; for multiple time-point comparisons, Kruskal-Wallis with Benjamini-Hochberg correction. Significance at p or q ≤ 0.05.
- Viral kinetics and inflammation: SARS-CoV-2 NP+ cells peaked at 3 dpi, declined by 6 dpi, and were undetectable by 14 dpi. Iba-1+ macrophages/histiocytes were significantly elevated versus mock at 1, 3, and 6 dpi, peaking at 6 dpi.
- Epithelial proliferation: Marked, heterogeneous epithelial proliferation occurred in alveoli and peribronchiolar regions. Affected lung area by epithelial proliferation: up to 1.3% at 3 dpi; 9.3–39.3% at 6 dpi; and 2.1–7.2% at 14 dpi. Cells exhibited atypia (karyomegaly, atypical mitoses).
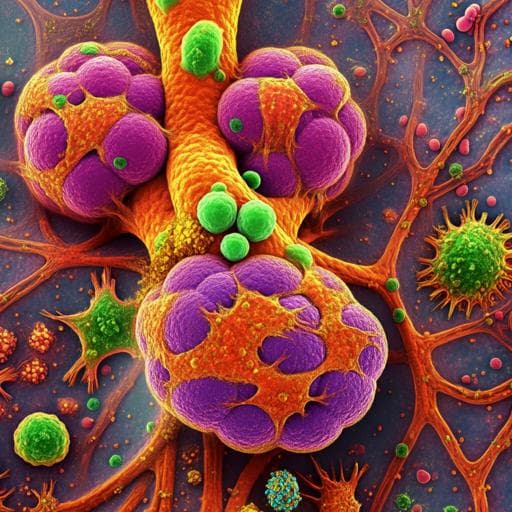
- ADI cells and AT2-ADI-AT1 trajectory: CK8+ ADI cells were abundant within proliferative foci at 3, 6, and 14 dpi, increased in both affected and non-affected alveoli. Double IF (proSP-C/CK8) showed transitional AT2→ADI states with morphology shifting from round to polygonal/elongated. At 6 dpi, proSP-C−CK8+ early ADI, proSP-C+CK8+ late ADI, and occasional elongated proSP-C+CK8+ AT1-like cells were observed; at 14 dpi, numerous early ADI persisted. CK8+ cells frequently exhibited nuclear TP53 at 6 and 14 dpi, indicating cell cycle arrest/DNA repair; no TP53 in rare CK8+ mock alveolar cells. TEM identified cells at alveolar edges with flattened AT1-like morphology yet retaining AT2 features (e.g., microvilli), consistent with ADI→AT1 transition.
- Human relevance: In three lethal COVID-19 ARDS samples, ADI cells (CK8 with proSP-C co-expression) were present and expressed TP53; in a non-COVID bronchopneumonia sample, ADI cells lacked TP53 co-expression, suggesting disease-specific ADI arrest in COVID-19.
- Airway progenitors in regeneration: CK14+ airway basal cells predominated in peribronchiolar proliferations at 6 dpi and migrated into alveoli. CK14+ cells increased in airways and alveoli at 3, 6, and 14 dpi. Double IF showed CK14+proSP-C+ cells (airway→AT2) and CK14/CK8 co-expression with morphological progression from cuboidal to elongated ADI-like cells (airway→ADI). SCGB1A1+ club cells were absent in early alveolar proliferates but increased by 14 dpi within peribronchiolar areas (up to ~40% of cells), often co-localizing with diminished CK14, indicating differentiation of CK14+ cells into club cells.
- Fibrosis and macrophages: At 14 dpi, 7/9 animals exhibited subpleural fibrotic foci with collagen deposition (Azan+) and α-SMA+ myofibroblasts; fibrotic area spanned 0.59–2.35% of lung. CD204+ M2 macrophages were increased versus mock at 3, 6, and 14 dpi and localized within/around fibrosis.
- scRNA-seq corroboration: At 5 dpi, clusters 2 and 6 (AT1/ADI) and partly 5 showed double expression of Rtkn2 and Lamp3 and high ADI marker module scores; at 14 dpi, clusters 2, 5, 7 (AT1/ADI) and clusters 0, 3, 9 (ADI) exhibited elevated ADI marker expression. Clusters with high ADI signatures showed increased module scores for p53 pathway and DNA repair, EMT, Wnt/β-catenin, Notch, and angiogenesis hallmark genes, supporting ADI persistence and involvement in pro-fibrotic/angiogenic microenvironments.
- Overall: Hamsters display ongoing alveolar regeneration beyond viral clearance with persistent ADI cells, airway basal cell contributions, M2 macrophage accumulation, and subpleural fibrosis, mirroring features reported in severe COVID-19 and offering a model for mechanisms underlying respiratory PASC.
The study addresses whether dysregulated alveolar regeneration, particularly persistence of ADI cells and aberrant progenitor responses, occurs after SARS-CoV-2 infection and could contribute to respiratory sequelae. Results demonstrate robust AT2→ADI→AT1 transitions with abundant CK8+ ADI cells persisting at 14 dpi, many exhibiting nuclear TP53 suggestive of senescence or prolonged cell cycle arrest. Ultrastructural evidence confirms ADI→AT1 progression, though atypical hypertrophic ADI cells likely fail to fully differentiate. Airway basal CK14+ progenitors mobilize into damaged alveoli, differentiating into AT2, ADI, and later club cells, paralleling human observations of basal cell ‘pods’ in COVID-19. scRNA-seq supports distinct and overlapping ADI/AT1 transcriptomic states and reveals enrichment of DNA repair, p53, EMT, Notch and Wnt/β-catenin signaling, and angiogenesis in ADI-rich clusters, consistent with mechanisms implicated in stalled differentiation and fibrotic remodeling. The presence of subpleural fibrosis with α-SMA+ myofibroblasts and persistent M2 macrophages suggests a pro-fibrotic milieu that may be driven by sustained inflammatory polarization and epithelial-mesenchymal pathway activation. Collectively, these findings indicate incomplete alveolar restoration post-infection, providing a mechanistic basis for impaired gas exchange and persistent respiratory symptoms in PASC, and establish the hamster as a translational model to interrogate and therapeutically target these processes.
SARS-CoV-2-infected Syrian golden hamsters exhibit persistent CK8+ ADI cells with TP53 activation, airway basal CK14+ progenitor contribution to alveolar repair, and subpleural fibrosis with M2 macrophage enrichment beyond viral clearance. Morphological, immunophenotypic, ultrastructural, and transcriptomic data converge to show dysregulated alveolar regeneration that parallels severe COVID-19 pathology in humans. This validates the hamster as a relevant model to study post-acute alveolar repair defects and to test interventions for PASC-related respiratory dysfunction. Future work should extend observation periods, perform lineage-tracing to definitively map cell origins/fates, evaluate lung function and gas exchange, and experimentally modulate implicated pathways (e.g., p53, Notch, Wnt/β-catenin) to restore proper ADI-to-AT1 differentiation and limit fibrosis.
- Specific AT1 immunolabeling in hamsters was unsuccessful (anti-AGER, -AQP5, -PDPN did not specifically label), precluding quantitative AT1 IHC and double-label demonstration of ADI→AT1; ADI→AT1 was inferred via ultrastructure.
- Clinical relevance of ADI persistence and fibrosis in animals was not directly assessed; longer-term studies with functional respiratory measurements are needed.
- Cell origin and fate interpretations (e.g., airway CK14+ basal cells to AT2/ADI/club; AT2 to ADI) rely on double-labeling and co-expression patterns; definitive lineage-tracing was not performed.
- scRNA-seq reanalysis may be limited by cell numbers and sequencing depth; some gene expressions or cell states with lower abundance may be underdetected; pathway activation inference requires protein-level validation and additional time points.
- Sex-based analyses were not performed (sexes pooled), potentially obscuring sex-specific differences.
Related Publications
Explore these studies to deepen your understanding of the subject.