Engineering and Technology
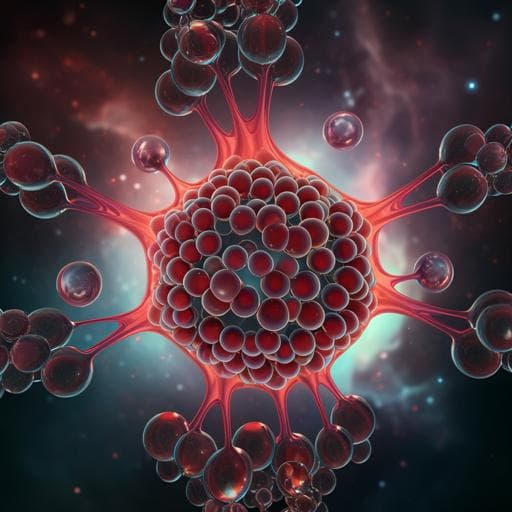
Generation of tumor spheroids using a droplet-based microfluidic device for photothermal therapy
J. M. Lee, J. W. Choi, et al.
This innovative study introduces a droplet-based microfluidic device capable of generating uniform cell spheroids at an impressive frequency of 70 Hz. Conducted by authors from Sogang University, this research showcases the device's potential in photothermal therapy for brain tumors and versatile applications in drug screening.
Related Publications
Explore these studies to deepen your understanding of the subject.