Medicine and Health
Development of a skin- and neuro-attenuated live vaccine for varicella
W. Wang, D. Pan, et al.
Discover the potential of v7D, a groundbreaking live-attenuated vaccine candidate for varicella, designed to minimize safety concerns while maintaining immunogenicity. Conducted by researchers including Wei Wang and Dequan Pan, this study showcases v7D's ability to replicate like wild-type VZV while significantly reducing infection in skin and neuronal cells.
Playback language: English
Introduction
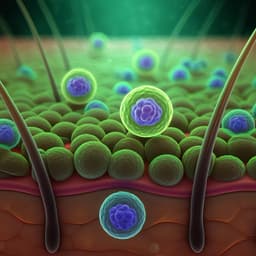
Varicella-zoster virus (VZV), the causative agent of varicella (chickenpox), poses a considerable global health burden, with millions of cases, severe complications, and deaths annually. While generally self-limiting, varicella can lead to life-threatening complications in immunocompromised individuals. Furthermore, VZV establishes latency after primary infection, potentially reactivating later in life as herpes zoster (shingles), sometimes accompanied by debilitating post-herpetic neuralgia. The currently used varicella vaccine, based on the live-attenuated Oka strain (vOka), has significantly reduced varicella morbidity and mortality. However, vOka retains neurovirulence and the capacity for latency and reactivation, raising safety concerns, including vaccine-associated varicella and herpes zoster. The vOka vaccine is a mixture of haplotypes, making its attenuation mechanism poorly understood and contributing to unpredictable outcomes. These safety concerns highlight the need for a safer, next-generation varicella vaccine. Advances in molecular virology and reverse genetics now allow the rational design of novel attenuated VZV vaccines. Specifically, ORF7 has been identified as essential for VZV virulence in skin and neuronal cells, while non-essential for replication in cell culture. This study focuses on the development and characterization of v7D, an ORF7-deficient, pOka-derived VZV vaccine candidate.
Literature Review
Existing literature extensively documents the global burden of varicella and the efficacy of the Oka strain varicella vaccine. Studies have highlighted the safety concerns associated with vOka, including the occurrence of vaccine-associated varicella and herpes zoster, linked to the presence of less-attenuated vOka haplotypes with differing skin and neurotropism. Research into the molecular mechanisms of VZV pathogenesis has identified key viral genes, particularly ORF7, involved in virulence and tissue tropism, providing a foundation for rational vaccine design. Previous research has shown that ORF7 is crucial for VZV replication in human skin and neurons, making it an attractive target for attenuation. However, the precise mechanisms by which ORF7 contributes to VZV virulence and tropism require further investigation. Studies utilizing SCID-hu mouse models and in vitro assays have been critical in understanding VZV pathogenesis and in preclinical vaccine evaluation, aiding in characterizing the tropism and pathogenicity of VZV and its mutant strains.
Methodology
This study involved the construction and comprehensive characterization of the v7D vaccine candidate. First, an ORF7-deficient VZV-BAC clone (b7D-GFP) was created by introducing a stop-codon mutation into the ORF7 gene of a recombinant Oka virus BAC clone (brOka-GFP). The v7D virus was then rescued from the BAC clone. Next-generation sequencing was used to verify the genetic stability of v7D. The replication kinetics of v7D were compared to those of rOka, a fully complemented control, 7R (ORF7-rescued control), and vOka in MRC-5 cells, differentiated SH-SY5Y neuroblastoma cells (dSY5Y), primary human dermal fibroblasts (HDFs), and primary human embryonic keratinocytes (HEKs). Western blotting was used to analyze viral protein expression and markers of cell damage (PARP and caspase-3 cleavage), with cell viability assessed using a CCK-8 assay. To assess the ability of v7D to infect and replicate in immune cells crucial for VZV dissemination, the study evaluated v7D replication in human peripheral blood mononuclear cells (PBMCs) using flow cytometry, immunofluorescence, and quantitative PCR.
In vivo attenuation was assessed using guinea pigs and cotton rats, and more physiologically relevant SCID-hu mouse models carrying human skin and dorsal root ganglia (DRG) xenografts. In the SCID-hu models, the study used cell-free virus inoculum to reduce the influence of pre-existing viral components. Viral titers were measured by plaque assay, and immunohistochemistry (IHC) was used to assess viral protein expression and tissue damage. Quantitative PCR was used to measure viral genome copy numbers and gene transcripts in the DRG xenografts.
The immunogenicity of v7D was evaluated in vitro using human dendritic cell (DC)-based assays. Human monocyte-derived iDCs were exposed to v7D and vOka, and DC activation phenotypes (CD40, CD80, CD83, CD86), cytokine/chemokine production, and T-cell stimulatory capacity were assessed using flow cytometry, multiplex cytokine/chemokine array, T-cell proliferation assays (BrdU ELISA and CFSE dilution), and IFN-γ ELISPOT assays. In vivo immunogenicity was evaluated in mice, rats, rabbits, and guinea pigs following subcutaneous immunization with v7D or vOka. Antibody responses (IgG titers, neutralizing antibody titers, and IgG subclass distributions) were assessed by ELISA and plaque reduction neutralization test. Cell-mediated immune responses were evaluated using splenocyte cytokine stimulation assays and PBMC analysis.
Key Findings
The key findings of this study demonstrate that the v7D vaccine candidate exhibits a dual-attenuated phenotype, with significantly reduced replication in human skin and neuronal cells compared to vOka, rOka, and 7R while maintaining robust replication in MRC-5 cells and PBMCs. In vitro, v7D showed comparable viral protein expression to vOka in MRC-5 cells. However, in dSY5Y cells, HDFs, and HEKs, v7D demonstrated markedly impaired replication and significantly reduced cytopathic effects. Importantly, v7D retained infectivity for human PBMCs, suggesting its ability to elicit immune responses. In vivo, v7D demonstrated significantly reduced neurotropism in guinea pigs and cotton rats and failed to establish an initial lytic infection in SCID-hu DRG xenografts. In the SCID-hu skin xenograft model, v7D showed a severely skin-attenuated phenotype with no lesions observed. In vitro, v7D induced similar levels of DC activation and T-cell stimulatory capacity compared to vOka. In vivo, v7D elicited comparable antibody and cellular immune responses to vOka in mice, rats, rabbits, and guinea pigs, inducing a mixed Th1/Th2 response. Furthermore, preclinical toxicity studies in nonhuman primates demonstrated that v7D lacked neurovirulence after intrathalamic inoculation and was well-tolerated with no systemic toxicity following repeated subcutaneous administration. v7D also induced comparable anti-VZV antibody and IFN-γ responses in nonhuman primates.
Discussion
The findings of this study strongly support v7D as a promising safer varicella vaccine candidate. The dual attenuation in skin and neuronal cells, coupled with comparable immunogenicity to vOka across multiple animal models, including nonhuman primates, addresses the key safety concerns associated with the current vOka vaccine. The mechanism of v7D's attenuation is likely linked to the disruption of ORF7 function, impacting cell-to-cell fusion and viral spread in skin and neuronal tissues, but this warrants further investigation. The retention of v7D's replication capacity in PBMCs suggests its ability to elicit robust immune responses while minimizing the risk of pathogenic infection. The study's preclinical data pave the way for clinical trials to evaluate v7D's efficacy and safety in humans, aiming to achieve broader varicella immunity with reduced risk of vaccine-associated adverse events.
Conclusion
This study presents a comprehensive preclinical evaluation of v7D, a novel, rationally designed live-attenuated varicella vaccine candidate. v7D exhibits a dual-attenuated phenotype, showing significantly reduced replication in skin and neuronal cells while retaining immunogenicity comparable to vOka across multiple animal models, including nonhuman primates. The lack of neurovirulence and systemic toxicity observed in nonhuman primates significantly enhances v7D's safety profile compared to the current vOka vaccine. These findings strongly support the advancement of v7D into clinical trials to assess its efficacy and safety in humans. Future research should focus on elucidating the detailed molecular mechanisms of ORF7's role in VZV pathogenesis and on long-term safety monitoring in humans.
Limitations
While this study provides extensive preclinical data supporting the safety and immunogenicity of v7D, some limitations exist. The use of animal models for evaluating VZV immunogenicity is inherently limited due to the virus's strict human specificity. The results obtained in animal models may not perfectly reflect the immune response in humans. Although the SCID-hu model offers a more physiologically relevant system, it still doesn't fully capture the complexity of human immune responses. Long-term safety data in humans will be crucial to fully assess the potential for wild-type reversion, recombination, latency, and reactivation of the vaccine virus, and to uncover any unforeseen adverse events.
Related Publications
Explore these studies to deepen your understanding of the subject.