Medicine and Health
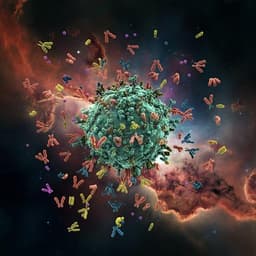
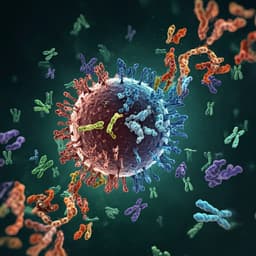
COVID-19 mRNA vaccine induced antibody responses against three SARS-CoV-2 variants
P. Jalkanen, P. Kolehmainen, et al.
This groundbreaking study reveals how the BNT162b2 mRNA COVID-19 vaccine induces robust antibody responses against various SARS-CoV-2 variants, including the concerning B.1.351 variant. Conducted by a team of esteemed researchers, the analysis shows that while neutralization capacity diminishes against B.1.351, a significant 92% of vaccinees still demonstrate protective antibody levels.
~3 min • Beginner • English
Related Publications
Explore these studies to deepen your understanding of the subject.