Medicine and Health
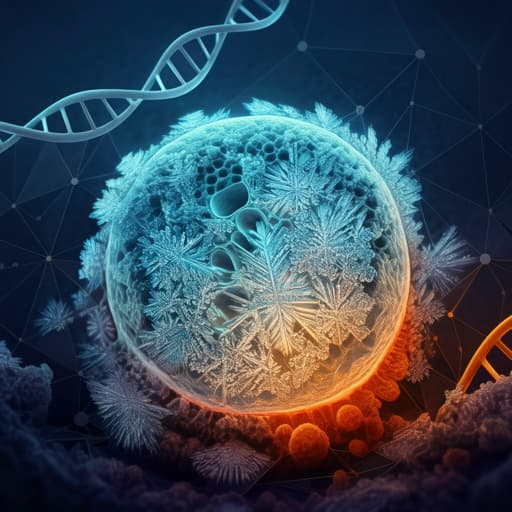
Clinical Medicine Only EBUS-Guided Mediastinal Lymph Node Cryobiopsy Enabled Immunotherapy in a Patient with Non-Small Cell Lung Cancer
J. Hetzel, L. A. Mauti, et al.
Discover how EBUS-guided transbronchial lymph node cryobiopsy enabled comprehensive tumor characterization in a challenging case of metastatic non-squamous non-small cell lung cancer. This innovative approach revealed PD-L1 expression in all tumor cells, leading to the initiation of tailored immunotherapy. Research conducted by Jürgen Hetzel, Laetitia A Mauti, Jonas Winkler, Sabine Cardoso Almeida, Philip Jermann, Miklos Pless, Lukas Bubendorf, Peter Karl Bode, and Maik Häntschel.
Related Publications
Explore these studies to deepen your understanding of the subject.