Medicine and Health
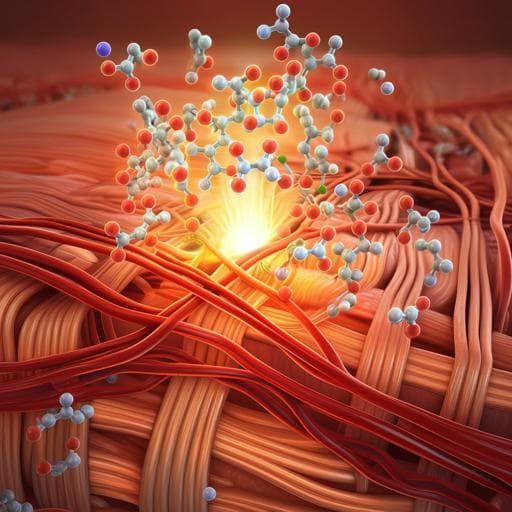
Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
Y. Yang, H. Wang, et al.
Discover how inflammation impacts tendon-bone healing and the potential of celastrol to regulate angiogenesis. This groundbreaking study, conducted by Yong Yang and colleagues, reveals insights into the mechanisms of healing following tendon injuries.
Related Publications
Explore these studies to deepen your understanding of the subject.