Medicine and Health
CD5L as a promising biological therapeutic for treating sepsis
L. Oliveira, M. C. Silva, et al.
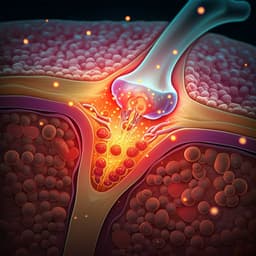
Discover the groundbreaking research by Liliana Oliveira and colleagues that unveils the therapeutic potential of CD5L in treating experimental sepsis. This study reveals how CD5L boosts neutrophil responses, enhances phagocytosis, and improves survival rates in mice, pointing towards a promising avenue for human treatments.
~3 min • Beginner • English
Introduction
The study addresses whether CD5 antigen-like (CD5L/AIM), a circulating SRCR-family protein that binds PAMPs and DAMPs and exhibits immunomodulatory functions, is protective or detrimental in sepsis. CD5L primarily circulates bound to IgM (biologically inert), with a free active fraction emerging in disease. Prior reports show both protective roles (e.g., enhancing macrophage survival during infection) and potential harm (e.g., promoting inflammation in atherosclerosis). CD5L can act as a PRR, opsonizing microbes and modulating inflammation. Sepsis is a leading cause of mortality worldwide and involves dysregulated inflammation. Clinical observations indicate elevated serum CD5L in sepsis patients, correlating with severity markers. The authors hypothesize that CD5L contributes to host defense in sepsis and that therapeutic administration of recombinant CD5L could improve outcomes by enhancing neutrophil responses, reducing pathogen burden, and dampening excessive inflammation. They test this in murine models of polymicrobial sepsis (CLP) and endotoxin-induced shock (LPS).
Literature Review
CD5L has been implicated across infections, cancer, and autoimmune diseases, with variable serum levels and assay inconsistencies complicating cross-study comparisons. Most circulating CD5L is IgM-bound and inactive under homeostatic conditions; during disease, a free active fraction emerges. CD5L displays anti-apoptotic effects, with context-dependent outcomes: protective in Listeria infection through macrophage survival and antimicrobial functions; detrimental in atherosclerosis via survival of foam cells and sustained inflammation. As a PRR, CD5L binds microbial PAMPs (LTA, LPS) and fungal components, potentially facilitating phagocytosis, similar to other SRCR proteins (SSC4D, SSC5D, DMBT1). It also exerts anti-inflammatory and tissue-repair roles by reducing pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), restraining Th17 pathogenicity, inhibiting inflammasome activation, and aiding debris clearance by binding DAMPs. Conversely, CD5L can worsen inflammation in some contexts (e.g., LPS-induced lung injury). In sepsis, prior clinical data show elevated serum CD5L in ICU sepsis patients, higher in septic shock and bacteremia, correlating with leukocytes, ALT, PCT, and SOFA scores. Experimental sepsis models (CLP and LPS) are widely used and enable comparative assessment of therapeutics, though each has limitations in mirroring human disease. A previous report suggested IP rCD5L at disease induction aggravated mortality, pointing to the importance of therapeutic timing and context.
Methodology
- Mouse models: Generated CD5L-deficient (Cd5l−/−) C57BL/6J mice via CRISPR/Cas9, inserting three stop codons and a frameshift in exon 3. Verified loss of circulating and peritoneal macrophage CD5L by ELISA and immunofluorescence. WT C57BL/6J mice served as controls.
- Sepsis models: Polymicrobial sepsis induced by cecal ligation and puncture (CLP). Mid-grade CLP: ligation at ~50% of cecum; high-grade CLP: ~75% ligation; both with 21G puncture. LPS-induced endotoxic shock: IP LPS 10 mg/kg (lethal) or 1.5 mg/kg (sublethal).
- Therapeutic intervention: Recombinant mouse CD5L (rCD5L; produced in HEK293T; endotoxin 0.21 EU/µg) administered IP or IV at 2.5 mg/kg (~50 µg/mouse) or 5.0 mg/kg. Treatment began 3 h post-CLP or LPS; second dose at 6 h post-CLP. PBS used as control. Safety assessed in naïve mice (clinical observation, AST, creatinine, histopathology).
- Experimental readouts: Survival up to 10 days (CLP) or 4–6 days (LPS); body weight loss; bacterial load (CFU) in blood, peritoneum, lungs, liver, kidneys; peritoneal leukocyte recruitment by flow cytometry (neutrophils CD45+CD11b+Ly6G+, macrophages CD45+CD11b+CD11c+F4/80+; M1/M2 markers Ly6C and CD206); cytokines/chemokines in peritoneal fluid and serum by multiplex bead assays and ELISA (e.g., IL-6, TNF-α, IL-17, CXCL1); organ injury markers (AST, creatinine); histopathology scoring (H&E) and HMGB1 immunofluorescence quantification; endotoxin (LPS) levels in serum by ELISA.
- Transcriptomics: Bulk RNA-seq of peritoneal cells from WT and Cd5l−/− mice at 0 h and 6 h post mid-grade CLP. Differential expression via DESeq2, pathway analysis by fGSEA (MSigDB hallmark sets), visualization by PCA and heatmaps.
- CD5L biodistribution and bioactivity: ELISA quantification of total CD5L in peritoneum and serum after CLP (WT) or after IV rCD5L in Cd5l−/− mice; correlation analysis of peritoneal vs serum levels. Size-exclusion chromatography and western blotting under non-reducing conditions to distinguish IgM-bound vs free CD5L; ELISA for total IgM.
- Phagocytosis assays: In vivo IP co-injection of pHrodo E. coli BioParticles with rCD5L (50 µg) in WT mice; ex vivo flow cytometry of peritoneal LPMs and neutrophils. In vitro: rCD5L-opsonized cecal bacteria (2 or 10 µg rCD5L) with thioglycolate-elicited macrophages (gentamicin protection assay). Ex vivo incubation of LPMs and elicited neutrophils with rCD5L-coated vs uncoated pHrodo particles over time.
- Neutrophil activation: Flow cytometric analysis of CD11b and Ly6G MFI on peritoneal neutrophils after IP or IV rCD5L in high-grade CLP, and in WT vs Cd5l−/− mice after mid-grade CLP.
- CXCL1 source and targeting: Chemokine arrays/ELISA in WT vs Cd5l−/− mid-grade CLP and in untreated vs IV rCD5L-treated high-grade CLP. In Cd5l−/− mice, IV rCD5L at 3 h post-CLP to assess rCD5L binding to peritoneal cell subsets and intracellular CXCL1 expression by flow cytometry.
- Statistics: Kaplan-Meier with log-rank test for survival; Mann-Whitney, unpaired t-tests with Welch’s correction, one-way/two-way ANOVA with multiple-comparison corrections as appropriate; t-SNE and LDA for integrative analysis.
Key Findings
- Endogenous CD5L is protective in sepsis:
- Cd5l−/− mice showed high susceptibility to mid-grade CLP: >60% mortality vs 0% mortality in WT; greater weight loss; markedly higher bacteremia and bacterial burden in lungs, liver, kidneys (~>10,000-fold more CFU in blood than WT at 72 h).
- Delayed leukocyte recruitment with significantly fewer neutrophils in peritoneum of Cd5l−/− vs WT; macrophage M1/M2-like proportions were similar.
- Multiplex cytokines indicated a slower inflammatory response in Cd5l−/−, especially evident at 72 h in peritoneum.
- RNA-seq of peritoneal cells at 6 h post-CLP: 507 genes upregulated and 133 downregulated in Cd5l−/− vs WT. Enriched pathways included IFN-α/IFN-γ responses, TNF-α signaling, IL-6/JAK/STAT3, hypoxia, apoptosis; oxidative phosphorylation pathways were downregulated, consistent with dysregulated inflammation typical of sepsis.
- rCD5L therapy dramatically improves outcomes in severe CLP:
- High-grade CLP with delayed treatment (3 h and 6 h): IP rCD5L yielded 55% survival; IV rCD5L achieved >70% survival over 10 days; untreated mice had low survival.
- Mechanistic correlates (IV vs IP):
- Neutrophil recruitment: peritoneal neutrophils increased within 3 h after first dose by ~4.5-fold (IV) vs ~2.6-fold (IP) relative to untreated.
- Systemic inflammation: IV rCD5L broadly reduced inflammatory cytokines in both peritoneum and serum; IP reduced cytokines mainly in peritoneum.
- Bacterial control: IV rCD5L reduced CFU in lungs and liver, and lowered blood CFU by >200-fold at 24 h; IP showed no significant CFU reductions across organs.
- Organ injury: Slight decrease in lung pathology scores and reduced serum AST with IV treatment.
- CD5L biodistribution and bioactivity:
- In WT mid-grade CLP, peritoneal CD5L protein rose sharply at 6 h and remained elevated; blood CD5L fell at 6 h and recovered by 24 h, suggesting redistribution to the infection site.
- In Cd5l−/− mice, IV rCD5L (2.5 mg/kg) at 3 h post-CLP led to detectable peritoneal rCD5L within 1 h, correlating with serum levels, confirming trafficking from blood to peritoneum.
- In healthy WT, >90% of CD5L is IgM-bound; during CLP, free peritoneal CD5L increased ~6-fold at 24 h. After IP or IV rCD5L, free (active) CD5L in peritoneum rose to levels comparable to IgM-bound CD5L, indicating bioactive availability; levels returned to baseline by 24 h.
- Phagocytosis and neutrophil function:
- In vivo, rCD5L did not change the fraction of LPMs or neutrophils that phagocytosed pHrodo E. coli particles, but suggested increased particle uptake per neutrophil.
- In vitro, rCD5L-opsonized pHrodo particles significantly increased neutrophil phagocytosis over 6–24 h; no enhancement of macrophage phagocytosis with rCD5L-opsonized cecal bacteria (gentamicin protection assays showed no increase).
- Anti-endotoxin and anti-DAMP effects:
- Cd5l−/− mice had higher circulating LPS at 72 h post-CLP than WT. After high-grade CLP, rCD5L (IP or IV) tended to reduce serum LPS at 24 h.
- HMGB1 (a DAMP) was increased in livers of Cd5l−/− vs WT after mid-grade CLP. In high-grade CLP WT mice, rCD5L reduced HMGB1 in lungs and liver (IP) and in liver and kidneys (IV).
- Protection from LPS-induced shock:
- Sublethal LPS (1.5 mg/kg): 73% mortality in Cd5l−/− vs 18% in WT over 6 days, indicating endogenous CD5L restrains endotoxin-driven inflammation.
- Lethal LPS (10 mg/kg): Untreated mice had 93% mortality by 2.5 days. rCD5L at 2.5 mg/kg improved survival to ~50%; at 5.0 mg/kg to ~78–80%.
- CXCL1-mediated neutrophil recruitment and activation:
- CXCL1 was consistently lower in Cd5l−/− vs WT after mid-grade CLP and higher in serum of IV rCD5L-treated vs untreated mice at 6 h post high-grade CLP.
- In Cd5l−/− mice given IV rCD5L, rCD5L bound multiple peritoneal subsets; only CD45− cells showed increased intracellular CXCL1 after rCD5L, implicating non-hematopoietic cells as CXCL1 sources.
- Neutrophil activation (CD11b upregulation) occurred rapidly (6 h) after IV but not IP rCD5L in high-grade CLP; WT neutrophils also showed higher CD11b vs Cd5l−/− in mid-grade CLP.
Discussion
The findings demonstrate that CD5L is a key regulator of host defense and inflammation during sepsis. Loss of CD5L compromises early neutrophil recruitment and bacterial control, leading to worsened outcomes in polymicrobial peritonitis. Transcriptomics of Cd5l−/− peritoneal cells revealed heightened pro-inflammatory and interferon signaling and reduced oxidative phosphorylation, aligning with dysregulated sepsis responses. Therapeutic rCD5L, particularly via IV administration after a clinically relevant delay, produced high survival in severe CLP by rapidly enhancing neutrophil recruitment and activation, lowering systemic cytokines, and reducing bacterial dissemination. The therapy also reduced circulating endotoxin and tissue DAMPs, supporting CD5L’s PRR-mediated neutralization and debris-clearing roles. Enhancement of neutrophil phagocytosis (but not macrophage phagocytosis) by rCD5L, together with increased CXCL1 production by non-hematopoietic cells and direct neutrophil activation (CD11b), provides a coherent mechanism: rCD5L augments CXCL1-driven chemotaxis and primes neutrophils, enabling swift local pathogen clearance and attenuation of systemic inflammation. The superiority of IV over IP likely reflects more effective activation of circulating neutrophils and systemic modulation. The robust protection in LPS-induced shock further substantiates CD5L’s anti-inflammatory efficacy independent of live pathogens. These results reconcile prior conflicting reports by highlighting timing: early co-administration may suppress beneficial initial inflammation, whereas delayed dosing dampens subsequent harmful hyperinflammation while supporting antimicrobial defenses.
Conclusion
This work establishes CD5L as a pivotal endogenous factor in sepsis and identifies recombinant CD5L as a highly effective therapeutic in murine models. IV rCD5L administered after sepsis onset increases free, bioactive CD5L at the infection site, elevates CXCL1, promotes neutrophil recruitment and activation, enhances neutrophil phagocytosis, reduces bacterial load, and decreases endotoxin and DAMP levels, culminating in markedly improved survival in severe CLP and lethal LPS shock. The combination of PRR-mediated neutralization of PAMPs/DAMPs and neutrophil-centric immune enhancement underlies its efficacy. Future research should optimize dosing, timing, and route, delineate the mechanisms by which CD5L induces CXCL1 in non-hematopoietic cells and directly activates neutrophils, evaluate long-term safety, and translate these findings into clinical trials to assess efficacy in human sepsis of diverse etiologies.
Limitations
- Disease models: LPS-induced shock lacks an infectious focus and CLP models primarily abdominal-origin sepsis; thus, findings may not generalize to all sepsis etiologies.
- Species/model constraints: Mouse responses (C57BL/6J) may not fully replicate human sepsis pathophysiology.
- Timing sensitivity: Therapeutic benefit depends on delayed administration; co-administration at disease induction may worsen outcomes (as reported by others).
- Mechanistic gaps: The precise signaling by which CD5L elevates CXCL1 in non-hematopoietic cells and directly activates neutrophils remains incompletely defined.
- Biomarker measurement: Standard ELISAs quantify total CD5L without distinguishing free vs IgM-bound; specialized methods were needed to infer bioactive fractions, which may limit broader assay comparability.
- Organ-specific effects: Reductions in HMGB1 and pathology were modest and organ-dependent; broader organ protection metrics warrant further study.
Related Publications
Explore these studies to deepen your understanding of the subject.