Medicine and Health
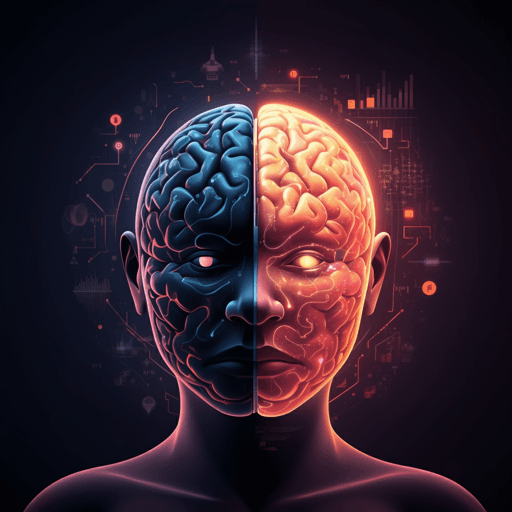
Can artificial intelligence improve the diagnosis and prognosis of disorders of consciousness? A scoping review
M. Bonanno, D. Cardile, et al.
AI (machine and deep learning) may transform how clinicians diagnose and prognosticate disorders of consciousness. This scoping review of 21 studies (14,683 patients, 180 controls) shows AI models using neurophysiology, neuroimaging, autonomic and clinical data to differentiate states (e.g., UWS vs MCS) and predict recovery, while calling for standardized data and demographic/etiological considerations. Research conducted by the authors listed in the <Authors> tag.
Related Publications
Explore these studies to deepen your understanding of the subject.