Medicine and Health
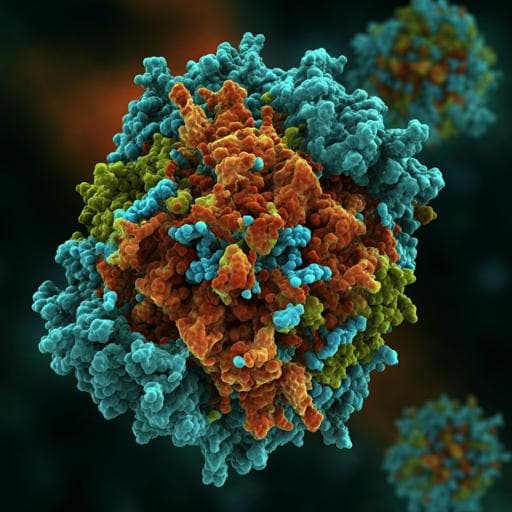
Broadly neutralizing antibodies against Omicron-included SARS-CoV-2 variants induced by vaccination
X. Chi, Y. Guo, et al.
Exciting research reveals that the adenovirus-vectored COVID-19 vaccine (Ad5-nCoV) induces broadly neutralizing antibodies against Omicron and other SARS-CoV-2 variants. The study introduces ZWD12, a monoclonal antibody with remarkable potency against these variants, paving the way for new therapeutic mAb drugs and innovative broad-spectrum vaccines. This groundbreaking work was conducted by a talented group of researchers.
Related Publications
Explore these studies to deepen your understanding of the subject.