Medicine and Health
A region-confined PROTAC nanoplatform for spatiotemporally tunable protein degradation and enhanced cancer therapy
J. Gao, X. Jiang, et al.
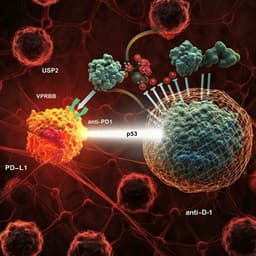
PROTACs catalytically degrade disease-causing proteins by recruiting E3 ligases to proteins of interest, offering potency at low doses and the potential to overcome resistance. However, clinical translation is challenged by suboptimal pharmacokinetics, insufficient tumor accumulation, and on-target/off-tumor toxicity. Prior strategies to enhance tumor specificity include ligand-directed conjugates (antibody-, folate-, aptamer-PROTACs), stimuli-responsive (photo-, radiation-, hypoxia-, enzyme-activatable) systems, and nanodelivery approaches. Tumor heterogeneity further complicates therapy; notably, cancer stem-like cells (CSCs) reside in hypoxic niches with low ROS, resist therapy, and drive relapse. Hypoxia-activated therapies can target CSCs but leave normoxic regions near vasculature undertreated. The study addresses this gap by designing a unified, region-confined nanoplatform that degrades BRD4 under both normoxic and hypoxic conditions, aiming to eradicate non-CSCs and CSCs concurrently.
The paper surveys tumor-targeted PROTAC strategies: ligand modifications (antibody-, folate-, aptamer-PROTACs), stimuli-responsive PROTACs (photolabile, radiation-triggered, hypoxia-responsive, enzyme-activatable), and nanosystem delivery (polymer encapsulation/covalent conjugation). It highlights tumor heterogeneity, the role of hypoxic CSCs in resistance and relapse, and the need for combinatorial or complementary mechanisms that simultaneously address normoxic and hypoxic tumor regions. Prior reports have identified BRD4 as a key oncogenic target and demonstrated hypoxia-activatable therapies for CSCs, but a single platform addressing both regions remained lacking.
Design and synthesis: ARV771 (BRD4-targeting PROTAC) was modified with a ROS-cleavable thioketal (TK) linker to yield ARV771-TK (ROS-activatable prodrug) and with an ethylene glycol linker to yield a ROS-inert control ARV771-Et. The ARV771-TK was copolymerized via RAFT with acid-responsive 2-(diisopropylamino)ethyl methacrylate (DPA) using a PEG-based chain transfer agent bearing an MMP-2-cleavable heptapeptide (GPLGLAG, GG), producing PGDT. A PPa-bearing copolymer (PGDA) for photodynamic ROS generation was synthesized by first making MPEG113-GG-b-P(DPA-r-HEMA) (PGDH) via RAFT then grafting PPa by esterification. Control polymers lacking GG or with ROS-inert ARV771-Et (PGDE) were also prepared and characterized (1H-NMR, MS, GPC). A hypoxia-responsive ARV771 derivative (ARV771-Nb, 4-nitrobenzyl masked VHL ligand hydroxyl) and hypoxia-inert ARV771-Ph were synthesized and validated by HPLC reduction assays. Nanoparticle assembly: Co-assembly of PGDT and PGDA yielded ROS-activatable, acid-labile nanoparticles (PGDAT). Encapsulating ARV771-Nb into PGDAT created dual-responsive PGDAT@N nanoparticles. Physicochemical characterization: DLS and TEM measured size/morphology; acid-triggered disassembly and PPa fluorescence restoration were quantified across pH; serum stability was assessed by DLS. Photoactivity and release: ROS generation quantified using SOSG/DCF probes under 671 nm irradiation at varying photodensities and pH. ARV771 release profiled by HPLC under irradiation (pH 7.4 vs 6.0) for PGDAT vs ROS-inert PGDAE. Cellular studies: MMP-2-mediated PEG deshielding assessed by pretreating nanoparticles with MMP-2 (0.2 mg/mL, 1 h) and measuring uptake in MDA-MB-231 cells by flow cytometry and CLSM. ROS production measured by DCFH-DA flow cytometry/CLSM under laser. BRD4 degradation was evaluated by western blot with/without irradiation and proteasome inhibition (MG132). Cytotoxicity evaluated by CCK-8 in MDA-MB-231 and CSC-enriched spheroids; tumor spheroid formation assays assessed CSC self-renewal. RNA-seq and qPCR in MDA-MB-231 and CSCs after ARV771 (1 µM, 24 h) evaluated DEGs/pathways (cell cycle, DNA replication, stemness), with validation of CDK4/6, p21, and stemness genes (Wnt7b, Sox4, Klf4, Rif1, Cdc73). In vivo biodistribution and activation: MDA-MB-231 xenografts received i.v. PGDAT or PDAT (PPa 5 mg/kg). Tumor accumulation assessed by photoacoustic imaging and IVIS; ex vivo organ/tumor imaging and CLSM (CD31 co-staining) evaluated penetration. Intratumoral ROS was probed with DCFH-DA following irradiation. Intratumoral ARV771 levels quantified by HPLC after free ARV771 or PGDAT ± laser (ARV771 dose 10 mg/kg). Antitumor efficacy: Orthotopic/subcutaneous MDA-MB-231 and HN30 HNSCC models were treated with PBS, ARV771, PGDA, PGDAT, PGDAT@N with standardized dosing (ARV771 10 mg/kg; PPa 5 mg/kg). Laser (671 nm, 400 mW/cm², 5 min) applied 36 h post-injection; 3 treatment cycles every 3 days. Tumor volumes, survival, body weight monitored. Mechanistic tissue analyses: H&E, TUNEL; IHC/IF and western blot of BRD4, CDK4/6, p21, cleaved caspase-3; CSC analysis by flow cytometry (CD44+/CD24−) and intracellular NANOG/SOX2/OCT4 staining. Hypoxia assessed by pimonidazole and HIF IHC. Region-confined activation imaging used hemicyanine probes (CY-TK and CY-Nb) formulated as PGDAC/PGDAC@N to visualize normoxic vs hypoxic activation in tumor sections.
- Chemistry and activation: ARV771-TK is ROS-activatable; ARV771 is regenerated upon PDT-generated ROS (HPLC/LC-MS). ARV771-Et is ROS-inert. ARV771-Nb is hypoxia-activatable (fully restored by Na2S2O4), while ARV771-Ph is inert. - In vitro BRD4 degradation: Free ARV771 degraded BRD4 in MDA-MB-231 cells with DC50 = 22 nM; ARV771-TK alone showed minimal degradation. In CSCs, ARV771 and ARV771-Nb degraded BRD4 dose-dependently with DC50 = 73 nM and 95 nM, respectively, downregulating CDK4/6 and upregulating p21; ARV771-Ph was inactive. - Nanoparticle behavior: PGDAT averaged ~65 nm at pH 7.4 (PDI < 0.2), disassembling at pH 6.0. PPa fluorescence increased ~6.0-fold at pH < 6.2 vs pH 7.4, confirming acid-induced disaggregation. ROS generation at pH 6.0 was up to 7.3-fold higher than at pH 7.4. Flow cytometry showed ROS increased 6.1-fold at 400 mW/cm² vs no irradiation. - MMP-2-triggered uptake: MMP-2-cleavable PGDAT showed 2.9-fold higher cellular uptake than MMP-2-inert PDAT after 24 h. - ROS-triggered release: At pH 6.0 with irradiation, PGDAT released ARV771 in a time-dependent manner; PGDAE showed negligible release across pH. - In vitro cytotoxicity: PGDAT alone weakly inhibited cells (~78% viability); PGDA + laser moderately inhibited (~63% viability); PGDAT + laser reduced viability to ~16% at 2.0 mg/mL. For dual-responsive PGDAT@N, laser enhanced killing >90% vs ~30% without laser and ~80% for PGDAT + laser. In CSCs, ARV771 and ARV771-Nb inhibited viability with IC50 = 0.42 µM and 0.57 µM and reduced spheroid numbers by ~90% and ~83% at 1.0 µM; ARV771-Ph had no significant effect. - In vivo tumor delivery/activation: PGDAT showed greater tumor accumulation than PDAT (1.7× PA signal and 1.9× IVIS fluorescence at 36 h). Ex vivo imaging and CLSM confirmed enhanced tumor penetration. Laser triggered strong intratumoral ROS. HPLC showed ARV771 concentration in tumors was 6.6× higher (vs PGDAT without laser) and 3.9× higher (vs free ARV771) for PGDAT + laser. - Antitumor efficacy (MDA-MB-231): Free ARV771 and PGDAT (no laser) showed negligible inhibition; PGDA + laser delayed growth (~50%); PGDAT + laser achieved ~80% regression and improved survival (~67% alive at day 36) with 1/6 complete responses but relapses occurred. CSC proportion increased after PDT (6.0× for PGDA + laser; 2.9× for PGDAT + laser), with elevated stemness markers and hypoxia. Dual-responsive PGDAT@N + laser achieved ~95% regression, 4/6 complete responses, and survival >80 days; PGDAT@N alone ~19% inhibition; PGDAT + laser ~80% with relapses. - Mechanism in vivo: PGDAT + laser and PGDAT@N + laser degraded BRD4 in tumors by ~65% and ~80%, respectively; CDK4/6 decreased; p21 and cleaved caspase-3 increased. PGDAT@N + laser reduced CSC fraction significantly (p = 0.0039) and downregulated NANOG/OCT4/SOX2. Region-confined activation imaging and IF showed BRD4 degradation in normoxia by PGDAT + laser, in hypoxia by PGDAT@N, and in both regions by PGDAT@N + laser. - Antitumor efficacy (HN30 HNSCC): PGDAT@N + laser eradicated tumors in 5/6 mice with survival >60 days; PGDAT@N alone ~34% inhibition; PGDAT + laser ~88% suppression with 3 relapses and 2 survivors >60 days. BRD4 degradation reached ~85% with concomitant CDK6 (−60%) and CDK4 (−50%) suppression and 5.0-fold and 4.3-fold increases of p21 and cleaved caspase-3, respectively.
The study demonstrates that a single nanoplatform can be spatiotemporally activated to degrade BRD4 across heterogeneous tumor microenvironments. MMP-2-triggered PEG deshielding enhances tumor accumulation and penetration. Acidic intracellular conditions restore PPa photoactivity, enabling ROS generation under 671 nm irradiation in normoxic regions; ROS cleaves TK linkers to release active ARV771 for BRD4 degradation, synergizing with PDT against non-CSCs. Concurrently, the hypoxia-responsive ARV771-Nb restores BRD4-degrading activity in hypoxic, CSC-enriched niches. This self-complementary design overcomes the limitations of single-modality approaches (e.g., hypoxia-only or ROS-only activation) by ensuring activation in both normoxic and hypoxic tumor zones. The result is superior tumor regression, reduced CSC populations, and prevention of relapse in breast and head–neck tumor models, while minimizing off-tumor effects via localized activation.
This work introduces a region-confined, ROS/hypoxia-activatable PROTAC nanoplatform that enables precise, spatiotemporally controlled BRD4 degradation in both normoxic and hypoxic tumor regions. Through MMP-2-mediated dePEGylation, acid-triggered photoactivation, ROS-driven PROTAC release, and hypoxia-activated PROTAC restoration, the platform achieves deep tumor penetration, robust BRD4 degradation, potent tumor suppression, and marked reduction of CSCs, preventing relapse in two tumor models. The strategy highlights a generalizable blueprint for integrating endogenous (e.g., MMP-2, hypoxia) and exogenous (e.g., light) stimuli for targeted protein homeostasis modulation. Future work may extend this design to other biomarkers (e.g., FAP, glutathione, esterases, cathepsin B, redox) and stimuli (e.g., X-ray, ultrasound, magnetic/electric fields) and leverage advances in fiber optics/endoscopic lasers to address clinical depth limitations of phototherapy.
- Dependence on external light activation limits tissue penetration depth, a known challenge for phototherapy; although fiber optics/endoscopic lasers may mitigate this, translation requires specialized delivery. - Efficacy relies on tumor-associated stimuli (MMP-2, acidic pH, hypoxia/NTR); variability across patients and tumor types may affect activation efficiency. - Results are from preclinical murine models (MDA-MB-231 and HN30); pharmacokinetics, safety, and efficacy in larger animals and humans remain to be established.
Related Publications
Explore these studies to deepen your understanding of the subject.