Medicine and Health
A modular self-adjuvanting cancer vaccine combined with an oncolytic vaccine induces potent antitumor immunity
K. Das, E. Belnoue, et al.
Explore cutting-edge research led by Krishna Das and colleagues, revealing how a novel combination of cancer vaccines can enhance immune responses against tumors, potentially overriding resistance to established therapies. This innovative approach harnesses the power of poly-functional T cells to optimize cancer treatment strategies.
~3 min • Beginner • English
Introduction
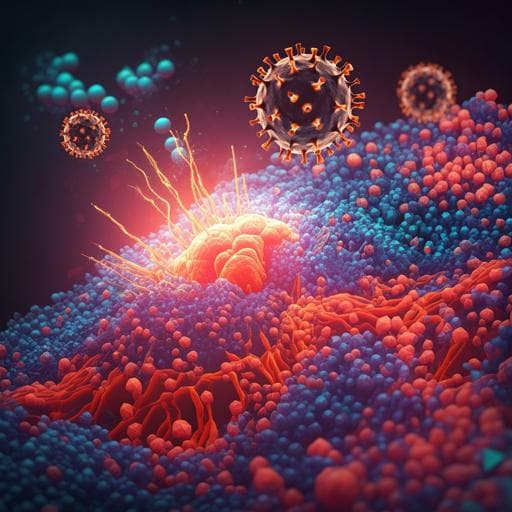
The study addresses how to enhance antitumor T cell responses and overcome immunosuppression in the tumor microenvironment to improve outcomes with immunotherapies, particularly in patients or tumor types that are nonresponsive to checkpoint inhibitors. The KISIMA platform is a modular, self-adjuvanting chimeric protein vaccine that integrates a multi-antigenic domain (delivering CTL and helper epitopes across HLA types), a cell-penetrating peptide for antigen delivery, and a TLR2/4 agonist for intrinsic adjuvanticity, generating robust and memory-prone T cell responses. Oncolytic viruses such as VSV-GP (VSV pseudotyped with LCMV-GP to reduce neurotoxicity) can induce inflammation, antigen release, and amplify immune responses but face tumor-intrinsic antiviral resistance and antiviral immunity that can limit efficacy. The rationale is that a heterologous prime-boost using KISIMA-TAA followed by VSV-GP-TAA could synergize by boosting tumor-specific T cells, shifting immunity from antiviral to antitumor, and remodeling the tumor milieu. The study systematically tests this concept across multiple murine tumor models and antigen classes, and evaluates synergy with checkpoint blockade.
Literature Review
Prior advances demonstrate clinical success of immune checkpoint inhibitors and adoptive cell therapies but with limited responses in many tumors due to immune exclusion and escape mechanisms. The KISIMA vaccine platform has shown induction of durable, memory-rich CTL responses via integrated TLR agonism and CPP-facilitated delivery. Oncolytic virotherapy provides multifaceted antitumor effects including immunogenic cell death, innate and adaptive activation, and potential in situ vaccination, yet clinical monotherapy performance often falls short due to antiviral immunity and tumor resistance. VSV-GP preserves lytic potency and broad tropism while mitigating neurotoxicity and has elicited strong adaptive responses as a vaccine vector. Heterologous oncolytic vaccination strategies have been proposed to tip the balance toward antitumor immunity and have shown promise in preclinical and early clinical testing, although mechanistic dissection has been limited. This work builds on these foundations to evaluate KISIMA and VSV-GP combinations, schedules, and routes, and their impact on T cell quality and the TME.
Methodology
- Study design: Preclinical evaluation of heterologous prime-boost vaccination combining KISIMA-TAA (subcutaneous) and VSV-GP-TAA (primarily intravenous; also intramuscular tested) in C57BL/6 mice. Comparisons included homologous regimens (KKK/KKKK and VVV/VVVV), alternate schedules (KVK, VKV), and routes (i.v., i.m., s.c., i.p.).
- Tumor models and antigens: Multiple syngeneic models with differing VSV-GP permissivity: E.G7-OVA (oncolysis-resistant), TC-1 (HPV E6/E7; IFN-restricted in vivo), B16-OVA (IFN-restricted), MC-38 (highly permissive in vitro but limited in vivo). Antigen cassettes included OVA (model), HPV-E7 (oncoviral), and neoantigens Adpgk and Reps1 (Mad24 construct).
- Vaccination regimens: Prime-boost schedules tested included KVK (KISIMA prime day 0, VSV-GP boost day 7, KISIMA boost day 14) and variants. Optimal regimen identified as KVK with VSV-GP given i.v. for maximal CD8+ T cell responses. Dosing details for checkpoint blockade: anti-PD-1 (200 µg i.v. twice weekly) or anti-PD-L1 (200 µg i.p.) per study schematics.
- Immunological assessments:
- Peripheral antigen-specific CD8+ T cells quantified by MHC multimer/tetramer staining over time in blood; memory precursor (CD127+) and effector (KLRG1+CD127−) phenotyping in blood, spleen, bone marrow at long-term time points (up to 19 weeks post-prime).
- Functional assays: Ex vivo restimulation with cognate peptides followed by intracellular cytokine staining for IFN-γ, TNF-α, CD107a degranulation, and granzyme B expression.
- Exhaustion/activation markers: PD-1, Tim-3, KLRG1 on antigen-specific CD8+ T cells in blood and tumors.
- Tumor microenvironment (TME) analyses:
- Flow cytometry of tumor-infiltrating leukocytes (CD45+) to profile T cells (CD8+, CD4+), myeloid subsets including M1/M2-like TAMs and MDSCs, and calculation of TAM-1/TAM-2 ratios.
- Immunohistochemistry (CD8) to assess spatial infiltration patterns within tumors.
- Transcriptomics: NanoString immune gene panel on tumor samples; differential expression versus mock; clustering, heatmaps, and pathway gene sets for cytotoxic T cells, cytokines, chemokines, dendritic cell function, and antigen processing/presentation; FDR adjustments by Benjamini–Yekutieli.
- Plasma cytokine/chemokine quantification (e.g., IFN-γ, CCL5, CXCL10, CCL2, IL-6, CXCL1, IL-1β) post-boost.
- Oncolytic activity assays:
- In vitro permissivity/lysis with and without IFN; in vivo viral activity kinetics including luciferase-reporter VSV-GP-Luc imaging following various primes (vehicle, KISIMA-OVA, KISIMA-HPV) to assess effects on intratumoral viral replication independent of TAA expression.
- Efficacy endpoints: Tumor growth (caliper; volume = 0.4×length×width^2), median survival, complete regressions, long-term survival. Re-challenge studies to assess memory in long-term survivors.
- Ethics and husbandry: Experiments approved by Austrian and Swiss authorities; standard housing conditions; humane endpoints defined.
Key Findings
- Immunogenicity and regimen optimization:
- KISIMA-TAA prime followed by VSV-GP-TAA boost (KV) elicited higher frequencies and numbers of circulating antigen-specific CD8+ T cells than the reverse order; a second KISIMA boost (KVK) further expanded OVA-specific T cells, whereas a second VSV-GP boost did not.
- Intravenous VSV-GP boost produced significantly higher antigen-specific CD8+ responses than i.m., i.p., or s.c.; i.v. VSV-GP within KVK yielded superior peripheral responses and long-lived memory precursors detectable in blood, spleen, and bone marrow up to 19 weeks.
- Heterologous KVK shifted the balance from antiviral to antitumor responses, reducing anti-VSV-N CD8+ T cells and increasing TAA-specific CD8+ T cells (inverse correlation observed). For HPV-E7, KVK induced >30-fold increase in circulating E7-specific CD8+ frequency over homologous regimens.
- Functionality and TME infiltration (TC-1 model):
- Despite similar intratumoral frequencies of E7-specific CD8+ T cells between KV and VV at the tumor site, KV priming yielded higher functionality: increased polyfunctionality (IFN-γ+TNF-α+CD107a+ triple-positive) in spleen and tumor, and more granzyme B+ CTLs.
- Intratumoral PD-1+Tim-3+ CD8+ T cells in KV mice retained KLRG1, indicating a less advanced exhaustion phenotype vs. VV.
- Tumor microenvironment remodeling and transcriptomics:
- KV vaccination upregulated 64.9% of panel genes vs. 36.8% with VV; 243 genes uniquely upregulated in KV, spanning innate and adaptive pathways. Thirty-five genes were uniquely downregulated in KV, including cancer progression-related Cdkn1a and Msln.
- KV enhanced signatures of cytotoxicity (Grzma/Grzmb/Grzmk, Prf1), dendritic cell activation and cross-presentation, cytokines (type I/II IFNs, Ifng, Tnf), chemokines, and antigen processing/presentation (including non-classical MHCs).
- Plasma cytokines/chemokines increased 1 day post VSV-GP-HPV boost in KV mice (IFN-γ, CCL5, CXCL10, CCL2, IL-6, CXCL1, IL-1β). Flow cytometry showed strong influx of CD8+ and CD4+ T cells and reduction of TAM-2, increasing TAM-1/TAM-2 ratio. IHC revealed deep intratumoral CD8+ infiltration after KV versus marginal localization in controls.
- Therapeutic efficacy across models:
- E.G7-OVA (oncolysis-resistant): All vaccine regimens delayed growth and improved survival, but marked regression of large established tumors occurred only with KVK after boost; circulating OVA-specific CD8+ levels correlated with regression.
- MC-38: Homologous VSV-GP-Mad24 (VVVV) achieved >50% complete regressions, indicating strong oncolytic component; KISIMA-containing regimens had lower efficacy despite robust T cell responses.
- TC-1: All vaccine schedules delayed growth and improved survival; circulating HPV-specific CD8+ were higher with KVK than VV, yet intratumoral frequencies were similar, aligning with comparable efficacy between VV and KVK alone.
- KISIMA prime was essential: VSV-GP-HPV treatment at day 14 post-graft induced complete remissions only when preceded by KISIMA-HPV prime, even in large tumors; virus-only treatment slowed growth without remissions. KISIMA prime did not increase intratumoral VSV-GP-Luc signal, indicating benefit was immune-mediated rather than via enhanced viral replication.
- Relapse biology and checkpoint synergy:
- At relapse, TC-1 tumors exhibited increased intratumoral exhaustion (PD-1+Tim-3+) and reduced CTL functionality; transcriptomes resembled mock/KK tumors with downregulation of cytotoxic, DC, and antigen presentation signatures and decreased cytokines/chemokines.
- Checkpoint inhibitors synergized with KVK: Anti-PD-1 alone was ineffective in E.G7-OVA and TC-1 but, combined with KVK, prevented relapse and produced many long-term survivors with median survival not reached. In MC-38, anti-PD-L1 alone delayed growth; combined with KVK yielded long-lasting complete regressions in >70% of mice.
- CPI increased circulating TAA-specific CD8+ T cells (OVA, Adpgk, HPV-E7) but did not expand antiviral VSV-specific CD8+ T cells; antitumor-to-antiviral ratios were not markedly altered by CPI addition.
- Re-challenge: Long-term survivors from KVK (+/− CPI) rejected re-implanted tumors efficiently, indicating durable memory; memory protection was lower after homologous VV in TC-1 and VV in MC-38 compared to KVK.
Discussion
The heterologous KISIMA-TAA prime and VSV-GP-TAA boost regimen addresses key barriers in cancer vaccination by increasing the magnitude and quality of tumor-specific CD8+ T cells and by converting immunologically cold tumors into inflamed, T cell–infiltrated lesions. KV/ KVK not only expands durable memory precursor pools but also produces polyfunctional CTLs with high cytotoxic potential, while simultaneously diminishing antiviral CD8+ responses that can otherwise dominate after viral vaccination. Transcriptomic and cellular analyses confirm broad activation of innate and adaptive pathways, enhanced antigen presentation, and reprogramming of the myeloid compartment toward an immune-supportive state. Importantly, benefits are observed even in models with limited in vivo viral propagation, indicating that oncolytic vaccination can potentiate antitumor immunity independently of sustained oncolysis. The approach sensitizes otherwise CPI-refractory tumors to PD-1/PD-L1 blockade, reducing relapses likely by curbing intratumoral T cell exhaustion and sustaining inflammatory signaling. These findings support heterologous oncolytic vaccination as a strategy to enhance CPI responsiveness and achieve durable control across diverse antigen contexts.
Conclusion
This work demonstrates that a modular, self-adjuvanting KISIMA cancer vaccine combined heterologously with an oncolytic VSV-GP vaccine expressing the same tumor antigens elicits large, persistent, and polyfunctional tumor-specific CD8+ T cell responses, remodels the tumor microenvironment to favor immunity, and synergizes with checkpoint blockade to produce durable tumor control and memory. The regimen improves the antitumor-to-antiviral T cell balance and can sensitize CPI-resistant tumors. Future research should prioritize clinical translation of the KV/KVK regimen, optimization of timing/routes and antigen payloads, deeper mechanistic studies of myeloid and CD4+ T cell contributions to TME repolarization, identification of biomarkers predicting response (e.g., permissivity, cytokine signatures), and exploration of combinations with additional immunomodulators to sustain intratumoral activation and prevent relapse.
Limitations
- Preclinical murine models with model antigens (OVA) and specific TAAs (HPV-E7, selected neoepitopes) may limit generalizability to human cancers with heterogeneous antigen landscapes.
- Some analyses were performed once or with small group sizes for certain endpoints, potentially affecting robustness; NanoString was limited to a predefined immune gene panel.
- Variable tumor permissivity to VSV-GP complicates attribution of efficacy to oncolysis vs. immune mechanisms; in vivo viral replication was generally limited and single-dose efficacy did not always translate from in vitro permissivity.
- Intratumoral T cell frequencies sometimes did not mirror peripheral expansions, suggesting trafficking or local suppression nuances not fully dissected.
- Long-term safety, optimal dosing, and potential toxicities of systemic VSV-GP in combination with KISIMA were not comprehensively evaluated here.
- Exact mechanisms by which KISIMA priming enhances subsequent viral boost effects (beyond T cell priming) and the role of CD4+ T cells and myeloid subsets require further study.
Related Publications
Explore these studies to deepen your understanding of the subject.